1st Trimester Bleeding: Ectopic Pregnancy – Diagnosis
Obstetrics and Gynecology
Context
- 2% of all pregnancies.
- Occurs in up to 18% of ED 1st trimester patients presenting with bleeding +/- abd pain.
- 9% of all pregnancy-related deaths and leading cause of maternal death in the 1st trimester.
- Abdominal pain and/or bleeding in the 1st trimester = ectopic pregnancy (EP) until proven otherwise.
- 30% of patients presenting with bleeding and/or pain in the 1st trimester will have a pregnancy of unknown location (PUL).
- PUL includes:
- EP.
- IUP – spontaneous abortion.
- IUP – normal developing pregnancy.
- An approach to a “rule-out” ectopic includes:
- Localization of pregnancy on US.
- If PUL, risk stratification with serial β-hCG and TVUS until a diagnosis of IUP or EP.
- Balancing the risk of ruptured ectopic and the risk of ending a viable, desired pregnancy.
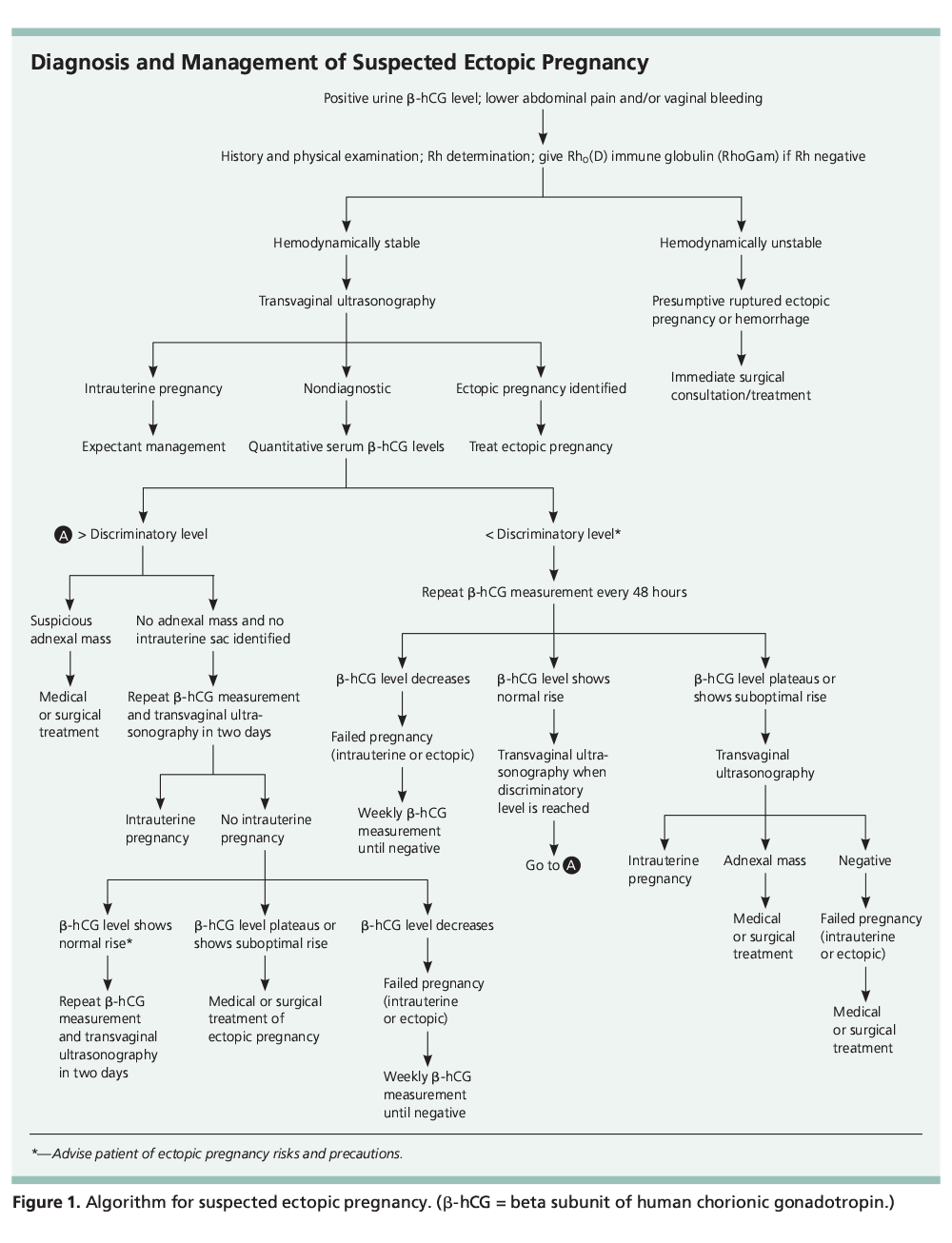
Diagnostic Process
- Classic triad: Pain (98%), amenorrhea (74%), and vaginal bleeding (56%).
- Ruptured ectopic:
- Hemodynamic instability.
- Peritoneal signs (rebound tenderness, cervical motion tenderness).
- May have normal vital signs and minimal tenderness.
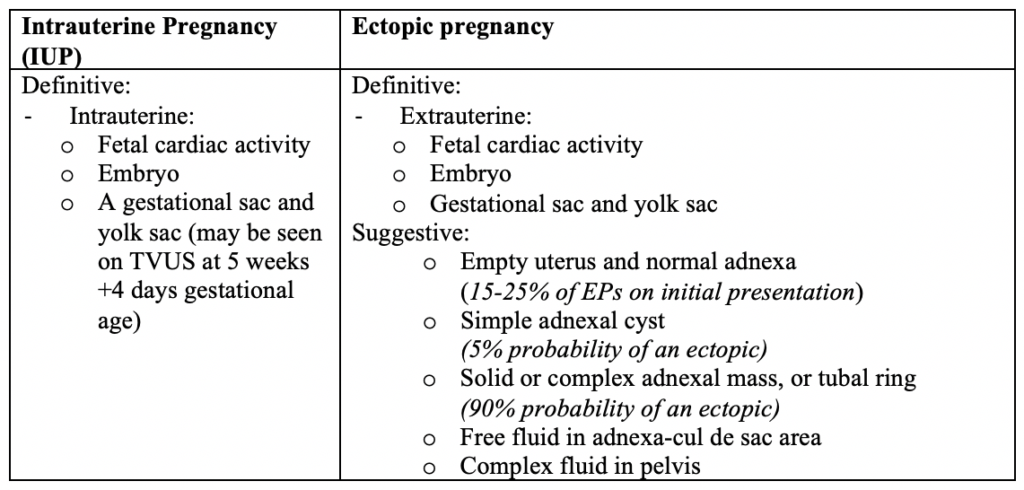
- Localize the pregnancy with transabdominal U/S, then transvaginal U/S if necessary.
- IUP visualization on ED POCUS effectively rules out an ectopic.
- Heterotopic pregnancies are rare, but considered with assisted reproductive technologies, as probability is higher (around 1%).
Criteria for localization of pregnancy on US:
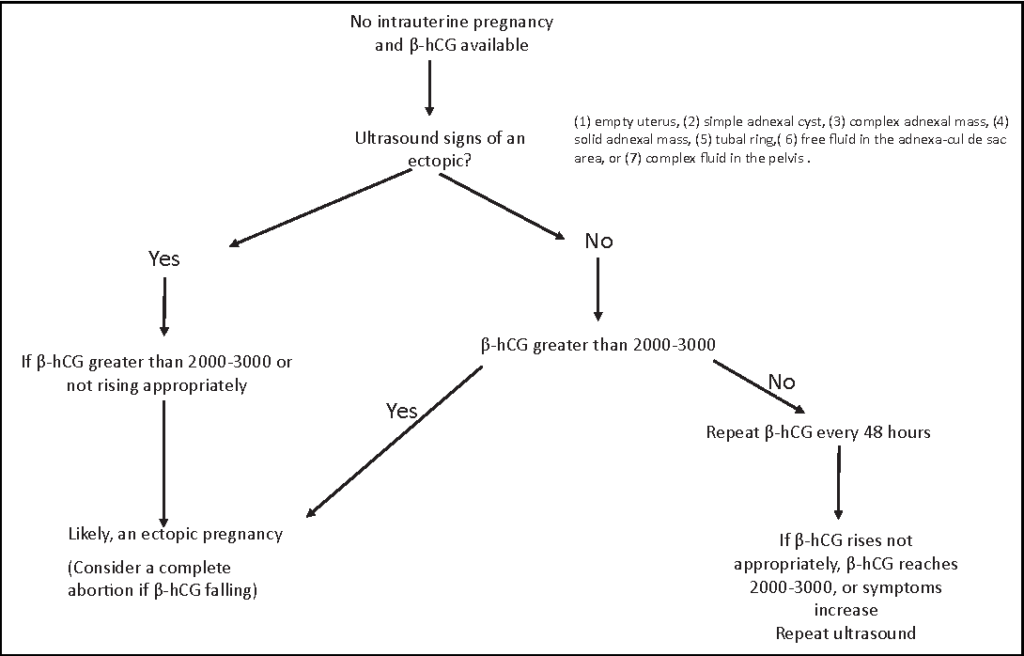
- If PUL, risk stratify using β-hCG:
- A discriminatory thresholds of β-hCG indicates when IUP usually can be seen on US but the utility of this threshold has been challenged. Most recent recommended thresholds are:
- Transvaginal US: β-hCG > 2000 – 3000 IU/L (especially before 7 weeks GA) OR the more conservative β-hCG > 3,500 IU/L suggested by American guidelines.
- Bedside abdominal US: β-hCG > 6,500 IU/L
- A β-hCG above the threshold and no IUP significantly increases the risk of ectopic.
- An EP can rupture at any β-hCG level.
- All symptomatic pregnant women presenting in the 1st trimester should have an US, irrespective of β-hCG.
- A discriminatory thresholds of β-hCG indicates when IUP usually can be seen on US but the utility of this threshold has been challenged. Most recent recommended thresholds are:
- If PUL, arrange an OB/GYN follow up and repeat β-hCG +/- TVUS in 48 hours.
- β-hCG should rise > 55% over 48 hours in the first 7 weeks.
- Failure to rise (falling or plateauing β-hCG) is indicative of a failing pregnancy (IUP or ectopic).
- Subsequent β-hCG measurements and TVUS should be obtained 2–7 days apart, depending on the pattern of change.
- The risk of rupture if there are no US findings of EP and no symptoms of rupture during diagnostic process is very low (0.03%). Therefore, there is limited risk in taking a few extra days to make a definitive diagnosis.
Common Pitfalls
- Relying on the classic triad of abdominal pain, vaginal bleeding, and missed menses to consider an ectopic.
- Not considering a heterotopic pregnancy in a high-risk population when there is an IUP.
- Not considering a ruptured ectopic pregnancy when a patient has already taken methotrexate.
- Assuming an ectopic is ruled out with a low β-hCG.
- Confusing a “double sac sign” in the uterus as an IUP, when it could be a pseudogestational sac or intrauterine cyst.
- Assuming no products of conception on U/S signifies a completed spontaneous abortion, rather than an ectopic.
- Failure to arrange adequate follow up if no IUP is seen and the U/S is indeterminate.
Resources
- Ectopic Pregnancy Scan Procedural Video
- Early Pregnancy EM Rounds Blog (St. John’s Regional Hospital, NB)
- Early Pregnancy Complications Podcast (emergencymedicinecases.com)
- POCUS for Vaginal Bleeding Blog (emergencymedicinecases.com)
- POCUS for 1st trimester bleeding (ACEP)
ALiEM Cards
- Ectopic diagnosis
- 1st trimester transabdominal ultrasound
- 1st trimester transvaginal ultrasound
- Methotrexate
Patient Resources
- Ectopic Pregnancy Patient Information Sheet (PHC and VCH)
- Ectopic Pregnancy (familydoctor.org)
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
All symptomatic pregnant women in the 1st trimester should receive a pelvic U/S, irrespective of β-hCG level.
Utility of a β-hCG discriminatory thresholds at 2000-3000 IU/L.
Related Information
Reference List
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Oct 16, 2020
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.