Achilles Tendon Rupture
Orthopedic
Context
- Peak incidence in those who are 30-40 years old. Affects athletes of all competition levels as well as sedentary patients. Other risk factors include fluoroquinolone antibiotics, steroid injections, and being a weekend warrior.
- Rupture may occur with sudden plantar flexion or dorsiflexion in a foot that is plantar flexed.
- Most tendon ruptures occur 2-6 cm above the insertion point, where the blood supply is poorest.
Diagnostic Process
- Many patients will feel as if they were violently kicked in the back of the ankle or calf.
- Some report a “pop” and experience acute, sharp pain in the region of the Achilles tendon.
- On physical exam, palpable defect in Achilles tendon and weak plantar flexion are common findings.
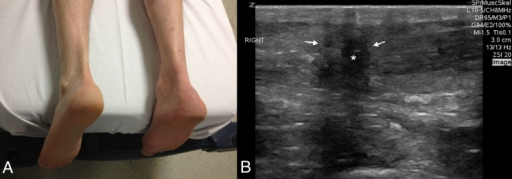
- Thompson Test or Simmonds Test or Calf Squeeze Test:
- Squeezing the calf should cause contraction of the Achilles tendon and plantar flexion.
- A POSITIVE TEST occurs when the Achilles tendon is completely ruptured and there will not be any apparent plantar flexion.
- Better to say test supports tendon rupture rather that positive or negative test.
- A patient with a complete tendon rupture may still be able to ambulate and have a relatively normal exam.
- Diagnosis of Achilles tendon rupture can often be made clinically.
- Imaging may be indicated. If doubt persists:
- Ultrasound can be useful to distinguish between complete vs. partial tears. Formal or bedside.
- MRI may be requested by ortho if surgical management is being considered.
- Plain radiographs taken to rule out other pathology.
Recommended Treatment
- Analgesics
- Splinting/bracing in resting equinus (foot planter flexed) position rather than neutral position:
- Walker boot with heel raises in place.
- Splinted in plantar flexion unless orthopedics wants cast.
- Non-weightbearing with crutches, and orthopedic opinion.
- There is a growing body of evidence showing equivalent functional results with both nonoperative management and operative repair.
- Indications for surgery include:
- Acute ruptures (<6 weeks)
- Complete tears
- Patients who wish to return to a demanding sport or heavy labor that increases risk for re-rupture.
- Local orthopedic culture will influence this.
- Physical therapy is critical for all patients to regain maximal ankle function.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
It remains unclear whether surgery versus nonoperative management will yield better outcomes, particularly with partial tendon rupture.
Related Information
Reference List
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Aug 16, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…



POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.