Acute Appendicitis
Gastrointestinal, Infections
First 5 Minutes
- Maintain a broad differential diagnosis – including ectopic pregnancy, ovarian/testicular torsion, bowel ischemia, ruptured AAA.
- Sick or not sick? Ensure patient is hemodynamically stable, manage with IV crystalloid or vasopressors if necessary, analgesia, may consider IV antibiotics empirically if appearing septic.
- Make patient NPO.
Context
- One of the most common causes of the acute abdomen.
- Cause is usually an obstruction of the appendiceal lumen causing inflammation of the appendiceal wall, which may be followed by localized ischemia, perforation, and the development of a contained abscess or generalized peritonitis.
- Most common abdominal surgical emergency globally, with a lifetime risk of 8.6% in males and 6.9% in females.
- Most common in patients aged 10-19 years, the most frequent cause of atraumatic abdominal pain in children >1 year old, most common non-obstetric surgical emergency in pregnancy.
Diagnostic Process
- Clinical Stratification Scoring: Alvarado Score for Acute Appendicitis, Samuel’s Pediatric Appendicitis Score (PAS) can help exclude acute appendicitis and identify intermediate-risk patients needing imaging.
- Presentation
- Symptoms: constant right lower quadrant abdominal pain, anorexia, nausea and vomiting.
- “Classic” presentation: periumbilical in nature with subsequent migration to the RLQ as inflammation progresses (migratory pain occurs only in 50-60%.)
- May have non-specific features, including indigestion, flatulence, bowel irregularity, diarrhea, generalized malaise.
- Physical examination
- Low-grade fever may be present (can be higher.)
- Tenderness in the right lower quadrant (RLQ.)
- McBurney’s point tenderness maximal tenderness at 1.5 to 2 inches from the anterior superior iliac spine (ASIS) on a straight line from the ASIS to the umbilicus.
- Rovsing’s sign pain in the right lower quadrant with palpation of the left lower quadrant.
- Psoas sign is associated with a retrocecal appendix. RLQ pain with passive right hip extension.
- Sensitivity is low (0.16-0.27) and specificity moderate (0.86-0.89) for these signs.
- Investigations
- WBC >10 often present but normal WBC and/or CRP does not rule out appendicitis.
- ~80% of patients have leukocytosis and a left shift.
- Imaging
- CT Abdomen/Pelvis is the preferred imaging evaluation in adults – with ultrasound and MRI reserved for pregnant women and children.
- CT scanning with contrast findings: enlarged appendiceal diameter >6 mm with an occluded lumen, appendiceal wall thickening (>2 mm), peri-appendiceal fat stranding, appendiceal wall enhancement, or appendicolith (~25% of patients.)
- The most accurate ultrasound finding is an appendiceal diameter of >6 mm.
Recommended Treatment
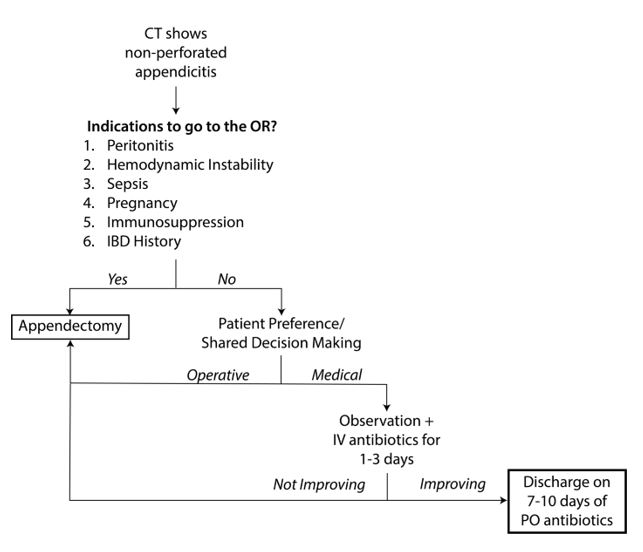
- Non-perforated appendicitis (simple or uncomplicated appendicitis) – 80% of cases.
- Usually surgical treatment but stable patients with can be treated with immediate appendectomy or initial nonoperative management based on local surgical preference.
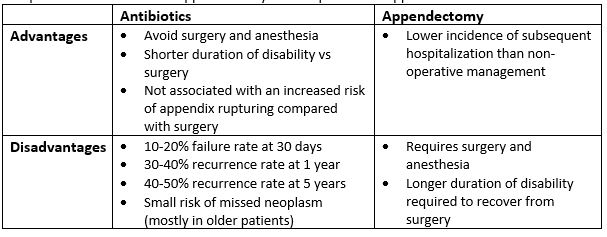
Comparison of antibiotics vs. appendectomy for non-perforated appendicitis.
Criteria For Hospital Admission
- All patients should initially be admitted hospital regardless of operative or non-operative management.
- In non-operative management, typically admit for 1-3 days of close observation.
Criteria For Transfer To Another Facility
- Consider transfer to another facility if there is no general surgery service/appropriate imaging available.
Criteria For Close Observation And/or Consult
- Consult General Surgery for early operative consult.
Criteria For Safe Discharge Home
- If non-operative management, may be appropriate to discharge home in 1-3 days after close observation and treatment with step down to oral antibiotics from intravenous.
- After appendectomy for simple – observe for diet tolerance.
- Most patients are discharged within 24 to 48 hours of surgery.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Low-moderate quality of evidence, based on observational studies, clinical experience, or from randomized, controlled trials with serious flaws.
Related Information
Reference List
Di Saverio S, Podda M, De Simone B. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World Journal of Emergency Surgery. 2020;15(1).
Martin RF, Kang SKKK. Acute Appendicitis in Adults: Diagnostic Evaluation [Internet]. UpToDate. 2021 [cited 2022Nov22]. Available from: https://www.uptodate.com/contents/acute-appendicitis-in-adults-diagnostic-evaluation?sectionName=IMAGING&search=appendicitis&topicRef=1386&anchor=H612714599&source=see_link#H612714599
Smink D, Soybel DISI. Management of Acute Appendicitis in Adults [Internet]. UpToDate. [cited 2022Nov22]. Available from: https://www.uptodate.com/contents/management-of-acute-appendicitis-in-adults#H9259945
Ward M, Visser R, Gillman LM. Dynamic practice guidelines for emergency general Surgery: Acute Appendicitis [Internet]. Acute Appendicitis: Dynamic practice guidelines for emergency general surgery. Committee on Acute Care Surgery, Canadian Association of General Surgeons; 2018 [cited 2022Nov22]. Available from: https://cags-accg.ca/wp-content/uploads/2019/07/ACS-Handbook-CPG-Ch-21-Abdominal-Wall-Reconstruction.pdf
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Oct 10, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.