Acute Limb Ischemia
Cardiovascular
Context
- More than 200 million people globally have lower extremity peripheral artery disease.
- Incidence of acute limb ischemia is 1.5 cases per 10,000 persons per year.
- High rates of morbidity and mortality, requires high index of suspicion for catastrophic outcomes:
- Despite urgent revascularization, amputation occurs in 10-15% of patients.
- 15-20% of patients die within 1 year after presentation.
- Definitions:
- Acute limb ischemia: sudden disruption of limb perfusion threatening limb viability, occurring within previous 2 weeks.
- Chronic limb ischemia: most commonly caused by PAD, gradually worsens over time, symptoms of claudication.
- Critical limb ischemia: limb pain that occurs at rest, can result in loss of tissue such as skin ulceration or gangrene.
- Signifies severely compromised limb perfusion, may be result of acute or chronic ischemia.
Diagnostic Process
- Risk Factors:
- Thrombosis: most likely to occur at site of atherosclerosis.
- Embolism: from heart or diseased artery.
- Hypercoagulability.
- Trauma.
- History of arterial interventions.
- History:
- Rule out other ischemic and non-ischemic causes of limb pain:
- Compartment syndrome, DVT.
- Trauma, gout.
- Focus on when symptoms started, which limb, events surrounding onset.
- Classic 6 P’s: absence of these symptoms does not rule out ALI.
- Pain
- Pallor
- Pulselessness
- Poikilothermia: impaired regulation of body temperature
- Paresthesia
- Paralysis: ominous sign
- ALI is not relieved by rest.
- Embolic source more likely: acute onset of ischemic symptoms in a previously asymptomatic patient with no history of claudication.
- Thrombotic source more likely: sudden worsening of symptoms in a patient with known history of claudication/peripheral vascular disease; more vague in onset.
- Rule out other ischemic and non-ischemic causes of limb pain:
- Physical Exam:
- Absence of pulses distal to occlusion but bounding pulses proximal to it.
- Lower limb pulses: femoral, popliteal, dorsalis pedis, posterior tibial.
- Upper limb pulses: brachial, radial, ulnar.
- Pale or cool skin.
- Motor and sensory exam might reveal weakness, decreased sensation.
- Absence of pulses distal to occlusion but bounding pulses proximal to it.
- Investigations:
- CBC, electrolytes, renal function, creatine kinase, coagulation profile.
- Imaging if appropriate: duplex ultrasound, CT angiography, MR angiography.
- CTA usually offers highest yield, with reconstruction invaluable for planning endovascular approach.
- Duplex ultrasound is less sensitive for detecting vascular pathology.
- ·Diagnostic approach:
- Evaluate pulses.
- If pulses not palpable, determine presence of flow with Doppler.
- If flow present, determine perfusion pressure proximal to Doppler probe using sphygmomanometric cuff (ABI).
- ABI is ratio of sBP of foot to highest brachial pressure in either arm.
- Normal ABI = 0.91 to 1.3
- Critical ABI = <0.4
- Classify ALI severity: Rutherford Classification
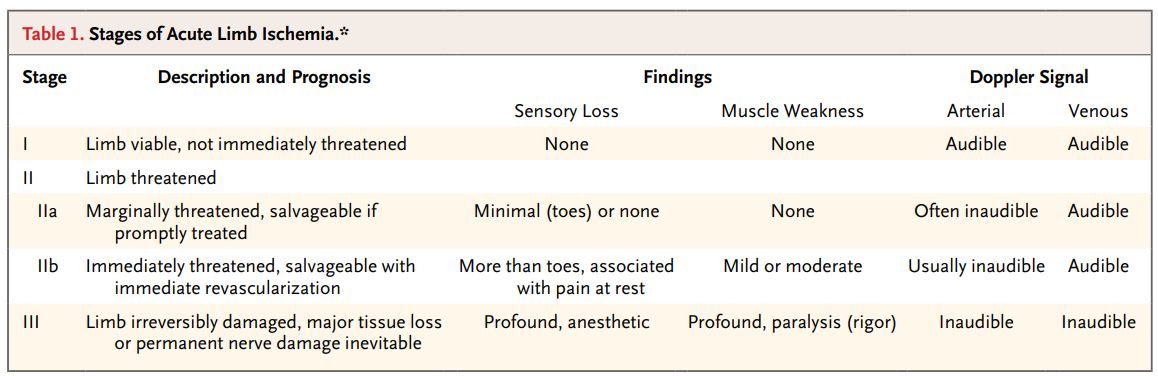
Image taken from Creager et al. Acute Limb Ischemia. N Eng J Med. 2012; 366: 2198-2206.
-
- Classification between stage I to IIA and IIB to III is important because mirrors. decision for an endovascular approach vs open surgical approach, respectively.
Management
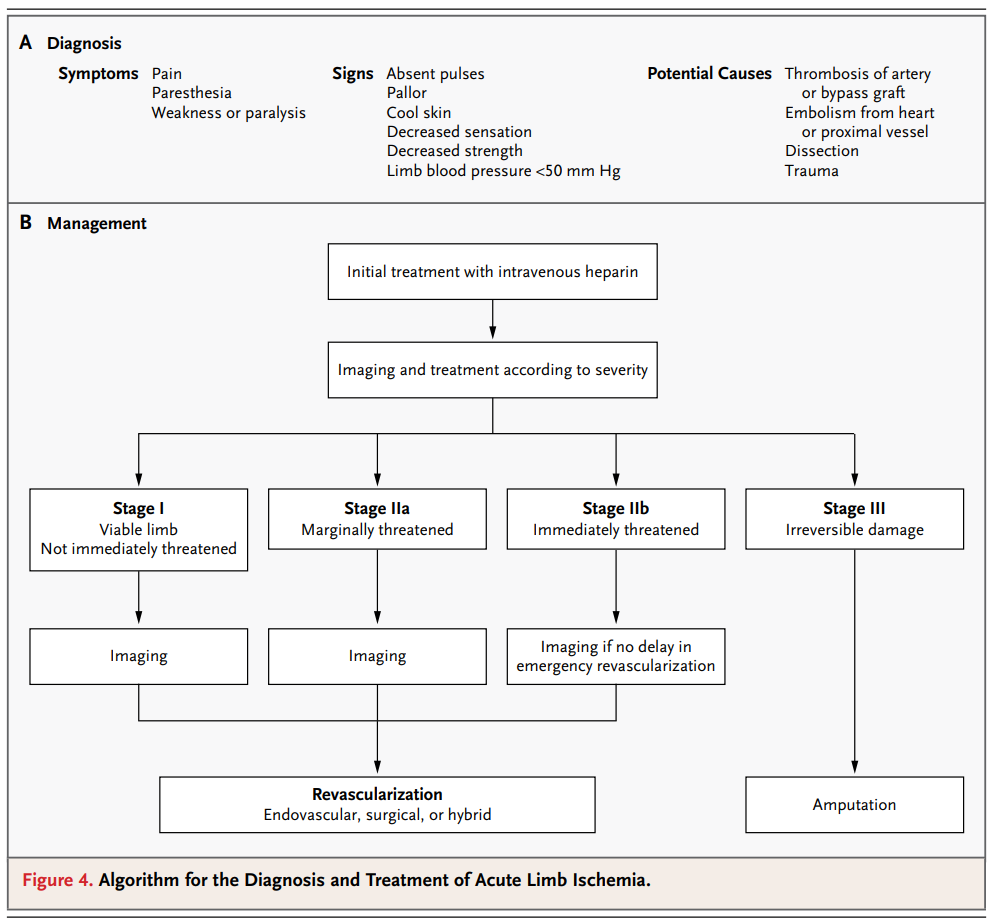
Image taken from Creager et al. Acute Limb Ischemia. N Eng J Med. 2012; 366: 2198-2206.
- Initial management:
- IV unfractionated heparin: dosing decision should be made with vascular surgery.
- Baseline recommendations: 80-150 U/kg bolus followed by infusion of 18 U/kg/hr to achieve PTT 2-2.5.
- Aspirin 325 mg PO.
- Keep patient in dependent position and warm the limbs.
- Pain control.
- Fluid resuscitation in hypovolemic patient.
- IV unfractionated heparin: dosing decision should be made with vascular surgery.
- Timing of intervention: <6 hours is optimal because patients presenting with >6 hr between symptom onset and intervention are 40x more likely to undergo amputation.
- Endovascular:
- Involves use of thrombolytics injected directly into thrombus over 12-24 hours, mechanical devices, or both to restore blood flow.
- Associated with higher rates of stroke and major hemorrhage within 30 days compared to surgical revascularization.
- Open surgical revascularization:
- Approaches include thromboembolectomy with balloon catheter, bypass surgery.
- Often requires subsequent operative intervention at 30 days.
- Associated with higher mortality in the elderly population.
- Long-term management:
- Warfarin for patients with thrombosis of native artery.
- DOACs may be considered in patients with embolism secondary to afib.
- Aspirin and/or clopidogrel for patients with thrombosis superimposed on atherosclerotic plaque: reduce risk of MI, stroke.
- Lifestyle management: smoking cessation, exercise, manage dyslipidemia.
- Clinical endpoint: disposition depends on severity of ischemia (see Rutherford Classification), etiology (embolic vs thrombotic), timing of symptoms, urgency for revascularization.
- All patients with ALI requiring surgical intervention should be admitted to hospital under the consultation of Vascular Surgery for immediate revascularization or amputation (if limb irreversibly damaged).
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Review articles and society recommendations, no RCTs.
Related Information
OTHER RELEVANT INFORMATION
ALiEM Card: http://aliemcards.com/cards/acute-limb-ischemia/
emDocs:http://www.emdocs.net/em3am-acute-limb-ischemia/
Emergency Medical Minute podcast: https://emergencymedicalminute.org/podcast-605-acute-limb-ischemia/
EM Takeaway: https://emtakeaway.com/em-case-acute-limb-ischemia/
Performing an ABI (St. Michael’s Hospital in Toronto): https://www.youtube.com/watch?v=0_0VlLSTAAE
Related Information
Reference List
Braun R, Lin M. Acute Limb Ischemia: A Case Report and Literature Review. J Emerg Med. 2015; 49(6): 1011-1017.
Creager MA, Kaufman JA, Conte MS. Acute Limb Ischemia. N Eng J Med. 2012; 366: 2198-206.
Kashyap VS, Gilani R, Bena JF, Bannazadeh M, Sarac T. Endovascular therapy for acute limb ischemia. J Vasc Surg. 2011; 53(2): 340-46.
McNally MM, Univers J. Acute Limb Ischemia. Surg Clin N Am. 2018; 98(5):1081-1096.
Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FGR, on behalf of the TASC II Working Group. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg. 2007; 45(1) Suppl:S5-S67.
Rutherford RB, Baker JD, Ernst C, et al. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg. 1997; 26:517-38.
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jan 19, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.