Approach to Flashes, Floaters, and Visual Field Deficits
Ears, Eyes, Nose, and Throat
Context
● Visual field disturbances include:
-
- Flashes (photopsia) – aberrant stimulation of the retina leading to the perception of flashing lights.
- Floaters – material in the vitreous body obstructing the light path leading to the perception of moving dark dots or strands.
- Visual field deficit – the partial or complete absence of light perception in a visual field.
● Coincident flashes and floaters increase the likelihood of a concurrent retinal tear.
● Retinal tear and retinal detachment are ophthalmologic emergencies.
Diagnostic Process
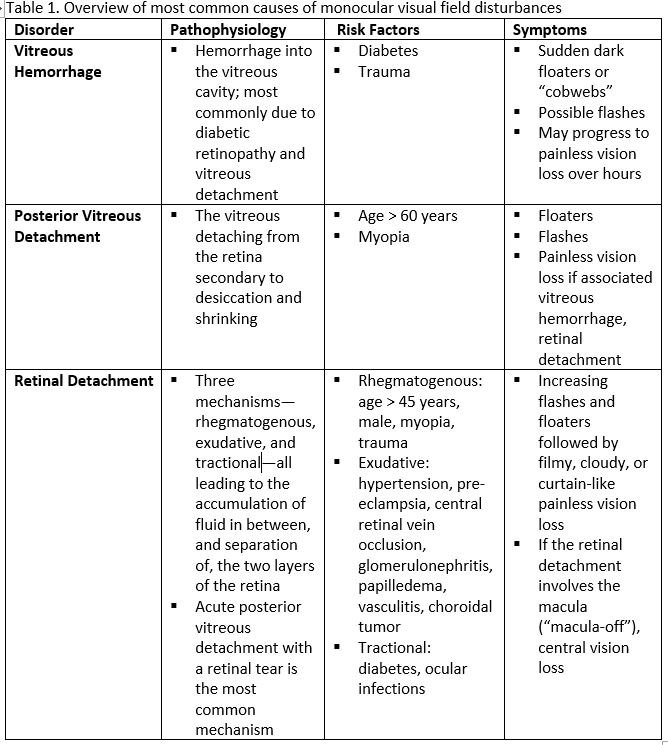
- The differential diagnosis of visual field disturbances can be categorized into monocular and binocular. Monocular disorders occur before the optic chiasm. The most common disorders include vitreous hemorrhage, posterior vitreous detachment, and retinal detachment, which are the focus of this PECS (see Table 1).
- Binocular disorders occur at or beyond the optic chiasm, and include migraines, scintillating scotomas, seizures, tumours, infarctions, arteriovenous malformations, and posterior reversible encephalopathy syndrome (referred to as chiasmal and cortical causes for the remainder of this PECS).
- History:
- Monocular or binocular
- Painful or painless
- Sudden or gradual
- Characteristics of the flashes and floaters
- Visual field(s) affected
- Loss of central vs peripheral vision
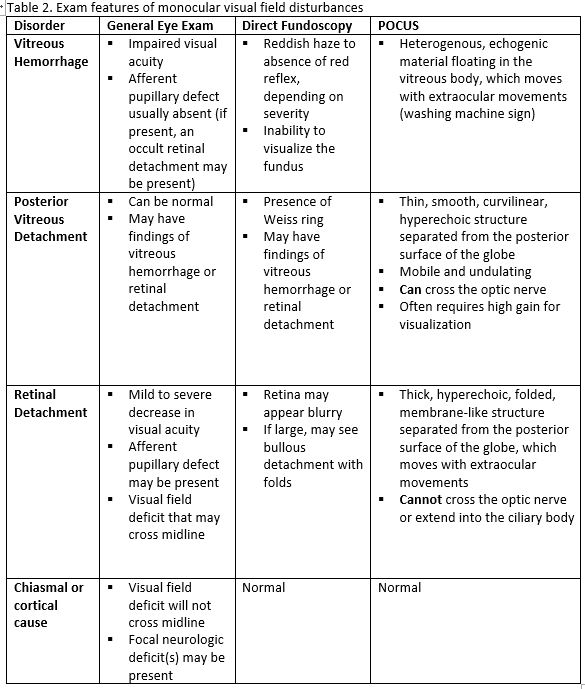
- Presence of neurologic symptoms
- Perform a complete eye exam, including visual acuity, visual fields, extraocular movements, pupil shape and reactivity, intraocular pressure, direct fundoscopy, slit lamp exam, and point-of-care ultrasound (POCUS; see Table 2).
- Direct fundoscopy has a low sensitivity and is technically difficult. As such, assuming provider comfort and accessibility, we recommend incorporating POCUS whenever possible while evaluating these ocular complaints.
- While POCUS has high sensitivity and specificity in the hands of a skilled operator, it is crucial to recognize our limitations as sonographers. Use ocular POCUS to help rule in an ophthalmologic diagnosis, but not to rule out critical diagnoses, such as retinal detachment, without ophthalmology consultation.
Vitreous Hemorrhage (The image is from The POCUS Atlas: Ocular Atlas, accessed Nov 10, 2022. They are licensed under the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International license.)
Posterior Vitreous Detachment (The image is from The POCUS Atlas: Ocular Atlas, accessed Nov 10, 2022. They are licensed under the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International license)
Retinal Detachment (The image is from The POCUS Atlas: Ocular Atlas, accessed Nov 10, 2022. They are licensed under the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International license.)
- If binocular, perform a neurologic exam. Neuroimaging will likely be indicated, but diagnostic workup is based on the underlying neurologic condition.
Red flags
- Sudden increase in floaters
- Photopsias
- Loss of vision, diffuse or focal (visual field defect)
- Recent eye surgery or eye trauma
- Eye pain
- Loss of red reflex
- Abnormal retinal findings
Recommended Treatment
- For vitreous hemorrhage and posterior vitreous detachment, urgent (24 to 48 hours) ophthalmology consultation is indicated.
- In general, vitreous hemorrhage and posterior vitreous detachment in isolation are managed non-pharmacologically, with activity limitation, stopping anticoagulants, and elevating the head of the bed.
- Risk of retinal tear is up to 70% in cases of posterior vitreous detachment with vitreous hemorrhage, thus ophthalmology assessment is crucial to guide ongoing management.
- However, if either condition is associated with the other, or with a retinal tear or detachment, surgery is often indicated.
- For retinal tear or detachment, immediate ophthalmology consultation and evaluation within 24 hours is indicated. Treatment may include surgery.
- For chiasmal and cortical causes, treat and consult according to the underlying etiology.
- Longstanding flashes and floaters require non-urgent referral
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
This resource is based on moderate-quality evidence from the emergency medicine literature and academic texts. When used by a skilled operator, POCUS has high sensitivity and specificity for retinal detachment.
Related Information
Reference List
Guluma K, Lee JE. Chapter 57: Ophthalmology. In: Walls RM, Hockberger RS, Gausche-Hill M, Erickson TB, Wilcox SR, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice, 10e. Elsevier; 2023:750-780.
Chesney GL, Vermeulen M. Chapter 39: Ocular Ultrasound. In: Soni NJ, Arntfield R, Kory P, eds. Point-of-Care Ultrasound, 2e. Elsevier; 2020:362-372. Accessed Jan 13, 2023.
https://www.clinicalkey.com/#!/content/book/3-s2.0-B9780323544702000392
Walker RA, Adhikari S. Chapter 241: Eye Emergencies. In: Tintinalli JE, Ma O, Yealy DM, Meckler GD, Stapczynski J, Cline DM, Thomas SH. eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 9e. McGraw Hill; 2020. Accessed Jan 13, 2023.
https://accessmedicine.mhmedical.com/content.aspx?bookid=2353§ionid=222404436#1166813220
Leveque T. Approach to the adult with acute persistent visual loss. In: Gardiner MF, Edlow JA, Ganetsky M, Givens J, eds. UpToDate. Waltham, MA: UpToDate Inc. Accessed Jan 13, 2023. https://www.uptodate.com/contents/approach-to-the-adult-with-acute-persistent-visual-loss?search=vitreous%20hemorrhage&source=search_result&selectedTitle=1~61&usage_type=default&display_rank=1#
https://www.cmaj.ca/content/184/4/431.short
https://www.sciencedirect.com/science/article/pii/S1568163715000343
https://www.racgp.org.au/afp/2014/april/flashes-and-floaters#ref-4
https://jamanetwork.com/journals/jama/fullarticle/184951
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jan 02, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.