Acute Respiratory Distress Syndrome (ARDS): Diagnosis & Initial Management
Cardinal Presentations / Presenting Problems, Critical Care / Resuscitation, Respiratory
Context
- ARDS is a life-threatening inflammatory condition of the lungs.
- Globally it affects 3 million patients annually and 10% of all ICU admissions.
- Triad of hypoxia, bilateral CXR opacities, and reduced lung compliance.
Pathophysiology
- Three phases: exudative, proliferative and fibrotic.
- Acute exudative phase = lungs initial response to injury and is characterized by the innate. inflammatory damage of alveolar endothelial and epithelial barriers allowing for the accumulation of fluid within the interstitium and alveolus.
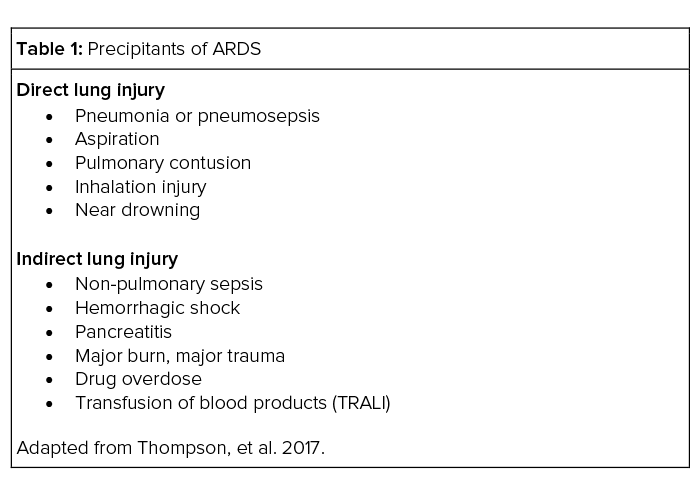
- Direct insults or indirect lung injury from systemic critical illness (Table 1).
Diagnostic Process
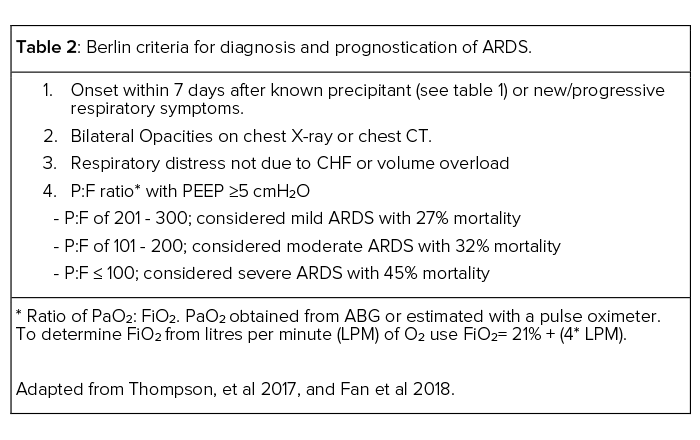
- The Berlin Definition (Table 2) is the most widely used clinical criteria.
- Consider common mimics of ARDS:
- Congestive Heart Failure
- Idiopathic pulmonary fibrosis
- Diffuse alveolar hemorrhage
- Drug-induced lung diseases
- Cancer
Recommended Treatment
- Supportive therapy is mainstay.
- Identification and treatment of the underlying cause.
- High flow nasal canula is preferential for management of mild ARDS. However, non-invasive positive pressure ventilation can also be used in some circumstances.
- For more severe cases, ventilatory support with mechanical ventilation continues to be the hallmark of ARDS management.
- Lung protective ventilation and the avoidance of ventilator-induced lung injury (VILI) are important principles in mechanical ventilation of patients with ARDS.
- Initial ventilator settings:
- Initial tidal volume (Vt): 6-8 mL/kg (ideal body weight)
- Target Plateau Pressure ≤ 30 cmH2O
- Permissive hypercapnia allowed to achieve above with goal pH ≥ 25
- A PEEP of at least 5 cmH2O should be used, and in more severe cases a higher PEEP should be used
- A more fluid restrictive resuscitation strategy is likely beneficial.
- Steroid use remains controversial. However, steroids should be used for COVID-19 related ARDS.
- For severe, refractory hypoxia related to ARDS:
- Optimization of PEEP
- Neuromuscular paralysis
- Prone positioning
- Institution of VV-ECMO
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Lung protective mechanical ventilation continues to be the hallmark of management in ARDS and is one of the few critical care interventions with a proven mortality benefit (Brower et al.)
Prone positioning for cases of severe ARDS is also well established (Proseva, Guerin et al 2013).
The diagnosis of ARDS using the Berlin Criteria has some degree of subjectivity leading to under recognition and inter-clinician variability.
Optimal methods for PEEP titration continues to be an evolving area in the literature, with no one standard accepted approach.
High flow nasal canula vs non-invasive ventilation. Evolving body of evidence and current recommendations are based largely on expert opinion and practice patterns.
Related Information
Reference List
Relevant Resources
RELEVANT RESEARCH IN BC
Sepsis and Soft Tissue InfectionsRESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Aug 04, 2021
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.