Amniotic Fluid Embolism
Critical Care / Resuscitation, Pregnancy
Context
- Amniotic fluid embolism (AFE) is an obstetric emergency of uncertain etiology, rapid onset, varying symptoms, and high fatality rate.
- The ‘classic’ AFE triad consists of hypoxia, hypotension, and coagulopathy.
- Most commonly a woman in labor or shortly after vaginal or caesarean delivery sustains acute dyspnea, desaturation, followed by sudden cardiovascular collapse. Commonly followed by cardiac arrest, coagulopathy, or both.
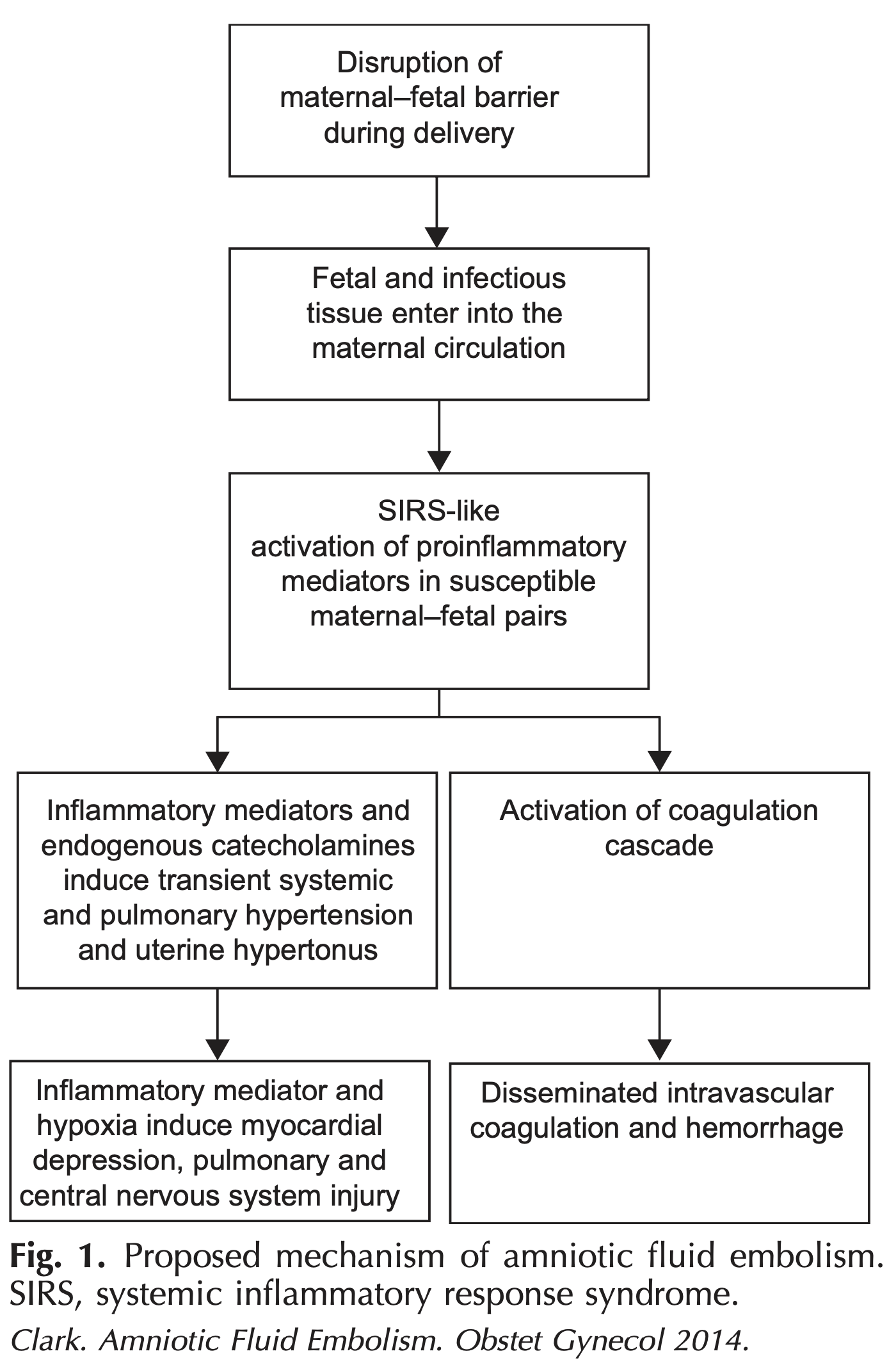
- No direct relation to either amniotic fluid or an embolism. The pathophysiology remains unclear, but is thought to be related to the entry of fetal antigens to maternal circulation which subsequently trigger an abnormal host response by activation of endogenous proinflammatory mediators.
- Both unpredictable and unpreventable with no identified demographic or clinical risk factor.
- Reported maternal mortality rate ranges from 20-60% depending on case inclusion criteria, with higher rates corresponding to more ‘classic’ presentations. Neonatal outcome mostly depends on maternal status, with fetal distress being common and mortality rates approaching 40% being reported.
Diagnostic Process
- The ‘classic’ AFE triad:
- Hypoxia
- Hypotension
- Coagulopathy
- Sudden onset during or immediately after labour.
- There are many atypical manifestations of AFE.
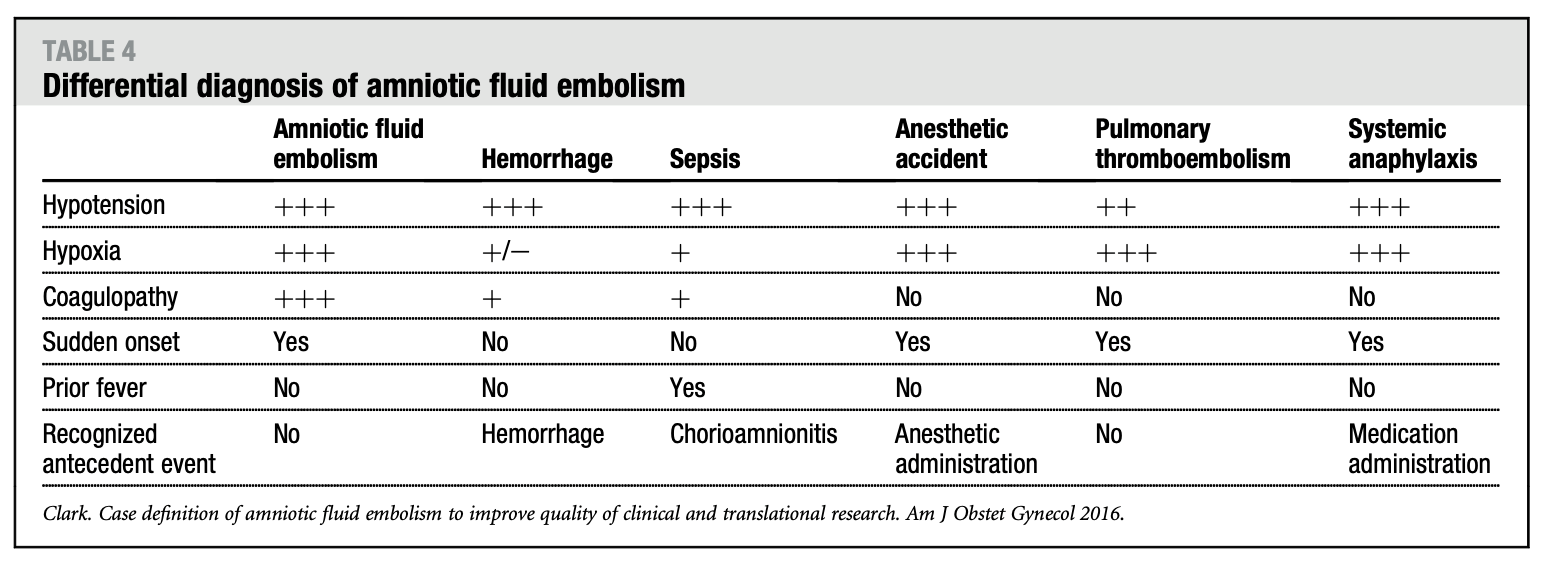
- At the present time AFE remains a clinical diagnosis and a diagnosis of exclusion.
- coagulopathy caused by (rather than the cause of) excessive bleeding, myocardial infarction, and other conditions can all resemble AFE.
Recommended Treatment
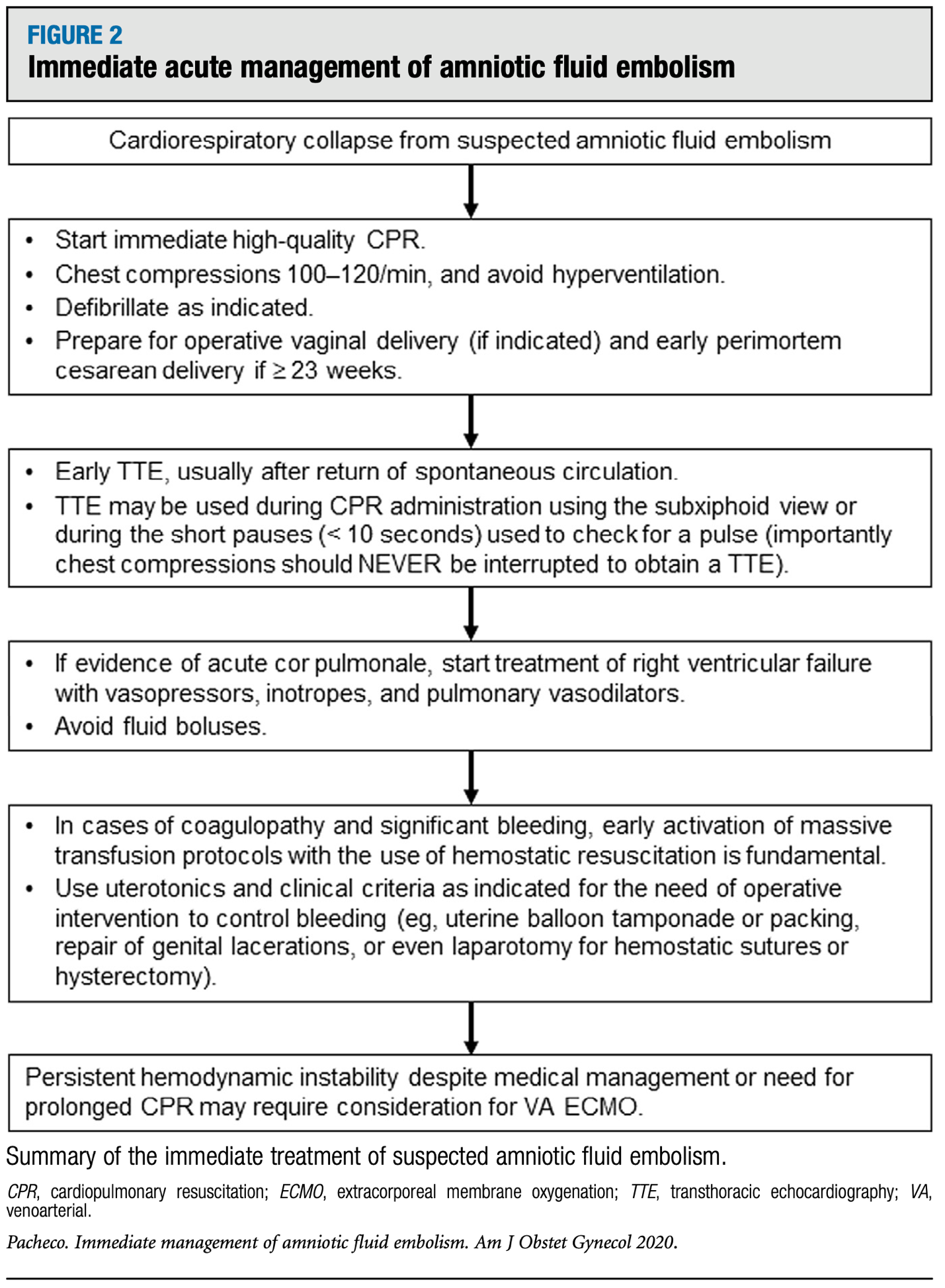
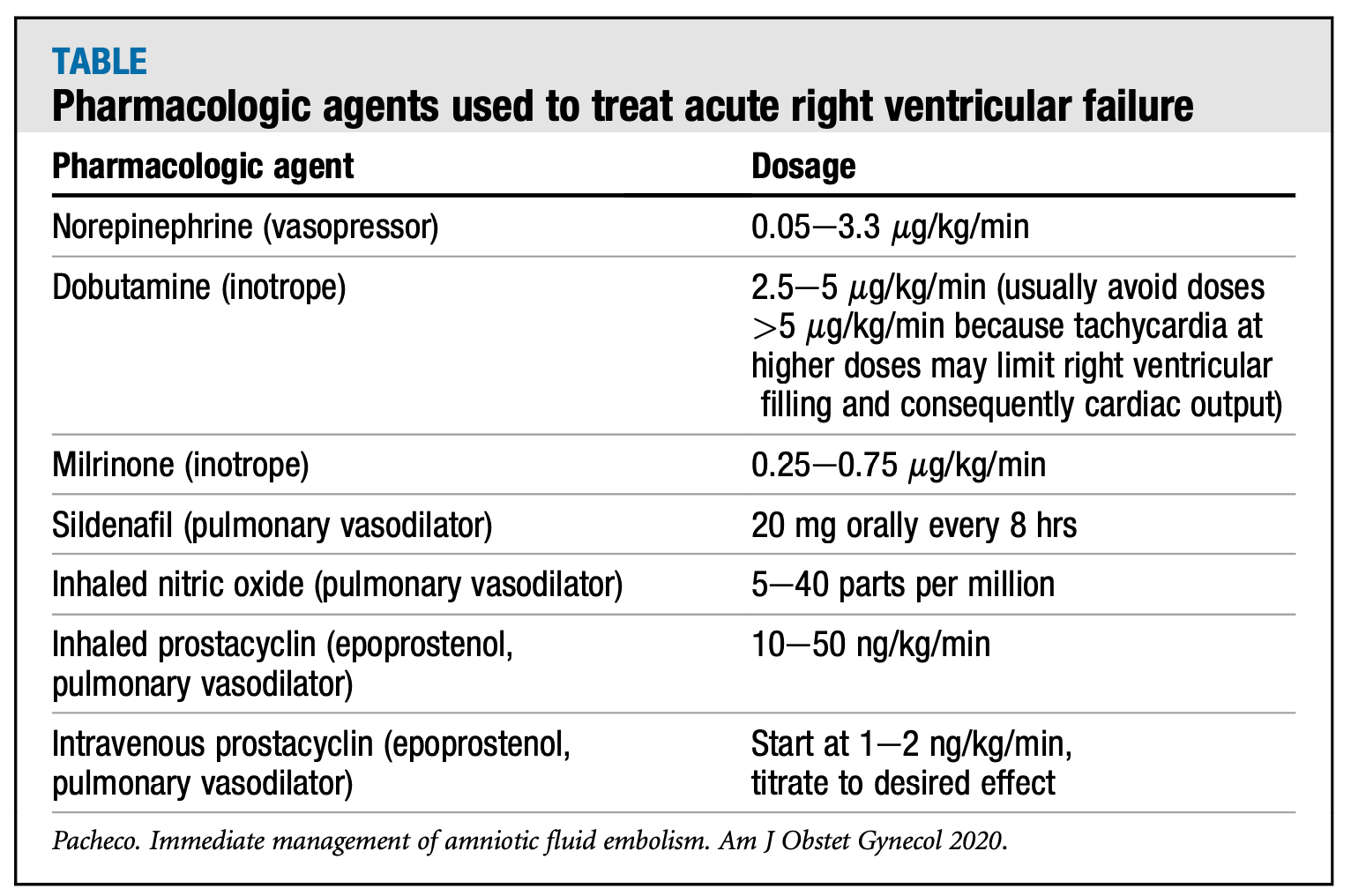
Treatment is primarily supportive and based on observable pathophysiology.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
The outlined approach to initial acute management of AFE is largely informed by the clinical opinions of those with experience in critical care obstetrics.
Related Information
Reference List
Clark SL. Amniotic fluid embolism. Obstetrics & Gynecology. 2014;123(2):337-348. doi:10.1097/aog.0000000000000107
Clark SL, Romero R, Dildy GA, et al. Proposed diagnostic criteria for the case definition of amniotic fluid embolism in research studies. American Journal of Obstetrics and Gynecology. 2016;215(4):408-412.
Combs CA, Montgomery DM, Toner LE, Dildy GA. Society for Maternal-Fetal Medicine Special Statement: Checklist for initial management of amniotic fluid embolism. American Journal of Obstetrics and Gynecology. 2021;224(4):B29-B32. doi:10.1016/j.ajog.2021.01.001
Fitzpatrick KE, van den Akker T, Bloemenkamp KW, et al. Risk factors, management, and outcomes of amniotic fluid embolism: A multicountry, population-based cohort and nested case-control study. PLOS Medicine. 2019;16(11). doi:10.1371/journal.pmed.1002962
Funk M, Damron A, Bandi V, Aagaard K, Szigeti R, Clark S. Pulmonary vascular obstruction by squamous cells is not involved in amniotic fluid embolism. American Journal of Obstetrics and Gynecology. 2018;218(4):460-461. doi:10.1016/j.ajog.2017.12.225
Lisonkova S, Kramer MS. Amniotic fluid embolism: A puzzling and dangerous obstetric problem. PLOS Medicine. 2019;16(11). doi:10.1371/journal.pmed.1002976
McDonnell NJ, Percival V, Paech MJ. Amniotic fluid embolism: A leading cause of maternal death yet still a medical conundrum. International Journal of Obstetric Anesthesia. 2013;22(4):329-336. doi:10.1016/j.ijoa.2013.08.004
Pacheco LD, Clark SL, Klassen M, Hankins GDV. Amniotic fluid embolism: Principles of early clinical management. American Journal of Obstetrics and Gynecology. 2020;222(1):48-52. doi:10.1016/j.ajog.2019.07.036
Pacheco LD, Saade G, Hankins GDV, Clark SL. Amniotic fluid embolism: diagnosis and management. American Journal of Obstetrics and Gynecology. 2016;215(2). doi:10.1016/j.ajog.2016.03.012
Salhi BA, Nagrani S. Chapter 178: Acute Complications of Pregnancy. In: Walls RM, Hockberger RS, Gausche-Hill M, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice. Ninth edition. Elsevier; 2017:2247-2248.
Related Information
OTHER RELEVANT INFORMATION
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jun 08, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.