C Difficile Infection
Gastrointestinal, Infections, Inflammatory
First 5 Minutes
- Thorough history is key. Broad differential diagnosis in patient presenting with abdominal pain and diarrhea, including:
- Acute abdomen.
- Other causes of infectious diarrhea.
- Non-infectious diarrhea, including osmotic, ischemic bowel, irritable bowel syndrome, inflammatory bowel disease, celiac disease, and microscopic colitis.
- Manage appropriately with IV crystalloid and vasopressors if necessary, IV antibiotics if patient appearing septic/toxic, hemodynamically unstable ideally targeting causative/suspected organism.
- Imaging of the abdomen and pelvis warranted for patients with clinical manifestations of severe disease/fulminant colitis to evaluate for toxic megacolon, bowel perforation, or other findings warranting surgical intervention.
- Suspect megacolon in patients with severe systemic toxicity together with radiographic evidence of large bowel dilatation (>7 cm diameter in the colon and/or >12 cm diameter in the cecum).
Context
- Clostridioides difficileis an anaerobic gram-positive, spore-forming, toxin-producing bacillus.
- Clostridioides difficile infection (CDI) is the most frequent cause of healthcare associated infectious diarrhea, and an emerging community pathogen causing significant morbidity and mortality.
- CDI can cause a spectrum of manifestations ranging from an asymptomatic carriage to fulminant disease with toxic megacolon.
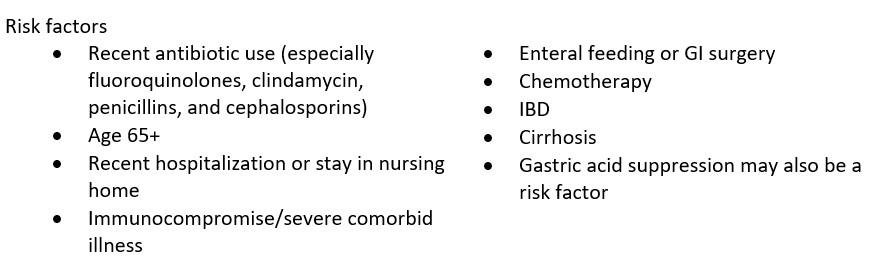
- difficile colonizes the human intestinal tract via the fecal-oral route (ingestion of spores) after normal gut flora has been disrupted (often in association with antibiotic therapy).
- Causative organism of antibiotic-associated colitis, including pseudomembranous colitis.
Diagnostic Process
- In British Columbia, the definition of a case of CDI is:
- Presence of diarrhea (e.g. three liquid or loose stools within a 24-hour period) or toxic megacolon (i.e. abnormal dilation of the large intestine documented radiologically) without other known etiology, AND laboratory confirmation of the presence of C. difficile toxin A and/or B (positive toxin, or culture with evidence of toxin production, or detection of toxin genes); OR
- Diagnosis of typical pseudo-membranes on sigmoidoscopy or colonoscopy; OR
- Histological/pathological diagnosis of CDI with or without diarrhea.
Presentation
- Non-severe disease: watery diarrhea is the main symptom. May also have lower abdominal pain and cramping, low grade fever, nausea, anorexia. May have some mucus or occult blood in stools.
- Severe colitis: diarrhea, lower quadrant or diffuse abdominal pain, abdominal distention, fever, hypovolemia, lactic acidosis, hypoalbuminemia, elevated creatinine, and marked leukocytosis.
- Fulminant colitis: hypotension/shock, ileus, or megacolon.
- Recurrent CDI: resolution of CDI symptoms while on appropriate therapy, with reappearance of symptoms within 2-8 weeks after treatment has been stopped.
Physical Exam
- Complete abdominal exam.
Investigations
- Diagnosis of CDI established via either a positive nucleic acid amplification test (NAAT) for C. difficile toxin B gene or a positive stool test for C. difficile toxins.
- Testing for C. difficile or its toxins should be performed only on diarrheal (unformed) stool, (Bristol Stool Chart type 6 or 7) unless ileus due to C. difficile is suspected.
- CT of the abdomen and pelvis with oral and intravenous contrast is the preferred imaging modality. Plain films may be useful for circumstances in which CT is not readily available.
- Endoscopy is not warranted in patients with typical clinical manifestations of CDI, a positive laboratory test, and/or clinical response to empiric treatment.
Recommended Treatment
- Infection control (contact precautions, hand hygiene).
- Discontinue use of inciting antibiotic agents.
- Supportive care (fluids, electrolytes as needed) and low-residue diet.
- Initial episode of nonsevere or severe CDI, appropriate treatment regimens include oral vancomycin or oral fidaxomicin.
- Fidaxomicin is favored over vancomycin given a small benefit with respect to recurrence rates, in accordance with 2021 Infectious Diseases Society of America (IDSA) guidelines, but currently has limited coverage in Canada.
- Metronidazoleis an alternative but less effective agent for treatment of nonsevere CDI if vancomycin is not available.
- Duration of initial antibiotic therapy for treatment of nonsevere CDI is 10 days, but should be individualized for patients with severe disease depending on response to therapy and clinical course.
- Avoid anti-motility agents like loperamide (Imodium) and diphenoxylate-atropine (Lomotil) when suspecting CDI given, although evidence for harm is equivocal.
- Early surgical consultation for patients with CDI who meet any of the clinical indicators associated with poor prognosis:
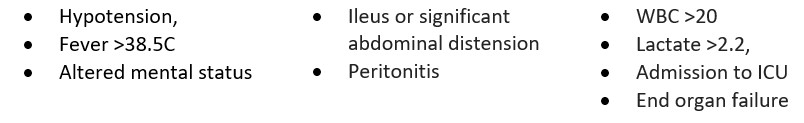
Criteria For Hospital Admission
Admit to hospital if patient is clinically deteriorating, septic/toxic appearing.
Criteria For Transfer To Another Facility
Generally no indication for transfer except in fulminant cases where ICU/critical care capabilities not available.
Criteria For Close Observation And/or Consult
Closely observe for any evidence of sepsis or clinical deterioration.
Criteria For Safe Discharge Home
Discharge home with adequate instructions for analgesia and antibiotic treatment if appropriate.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Evidence is moderate-high: based on Association of Medical Microbiology and Infectious Disease Canada treatment practice guidelines for Clostridium difficile infection, including four randomized trials.
Related Information
Reference List
CDI Working Groups of British Columbia. British Columbia Clostridium difficile Infection (CDI) Toolkit and Clinical Management Algorithm [Internet]. [cited 2022Nov28]; Available from: https://www.picnet.ca/wp-content/uploads/Toolkit-for-Management-of-CDI-in-Acute-Care-Settings-2018.pdf
Kelly CP, Lamont JT, Bakken JS. Clostridioides difficile infection in adults: Treatment and prevention [Internet]. UpToDate. 2021 [cited 2022Nov28]. Available from: https://www.uptodate.com/contents/clostridioides-difficile-infection-in-adults-treatment-and-prevention
Lamont JT, Kelly CP, Bakken JS. Clostridioides difficile infection in adults: Clinical manifestations and diagnosis [Internet]. UpToDate. 2022 [cited 2022Nov28]. Available from: https://www.uptodate.com/contents/clostridioides-difficile-infection-in-adults-clinical-manifestations-and-diagnosis?search=c+difficile+&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2
Loo VG, Davis I, Embil J. Association of Medical Microbiology and Infectious Disease Canada treatment practice guidelines for clostridium difficile infection. Official Journal of the Association of Medical Microbiology and Infectious Disease Canada. 2018;3(2):71–92.
McDonald LC, Gerding DN, Johnson S, Kelly C. Clinical practice guidelines for clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clinical Infectious Diseases. 2018;66(7).
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Dec 16, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.