Acute Kidney Injury – Diagnosis & Treatment
Urological
Context
- Acute Kidney Injury (AKI) is defined as an acute loss of kidney function, with subsequent accumulation of metabolic waste products.
- AKI can be divided into 3 subtypes:
- Prerenal – Decrease in kidney perfusion
- Intrarenal – Injury to kidney parenchyma
- Postrenal – Urine obstruction
- Clinical presentation of AKI is varied. Patients may be asymptomatic and be diagnosed incidentally on lab investigations or imaging, or present with overt signs and symptoms such as:
- Oliguria/anuria
- Pulmonary edema
- Evidence of shock
- Risk factors for AKI:
- >65 years old
- Volume depletion
- Surgical procedures
- Infections
- Nephrotoxic agents
- Hypertension
- Diabetes
- CHF
- Atherosclerosis
- Chronic Kidney Disease
- Obstructive uropathy
- Life threatening complications of AKI:
- Severe metabolic acidosis
- Hyperkalemia
- Pulmonary edema
- Recovery of kidney function may occur within days or require dialysis for many months depending on the severity, duration, and recurrence of the initial AKI.
- Patients may require admission to monitor for recovery of renal function, and nephrology or urology consultation for further workup and management.
Diagnostic Process
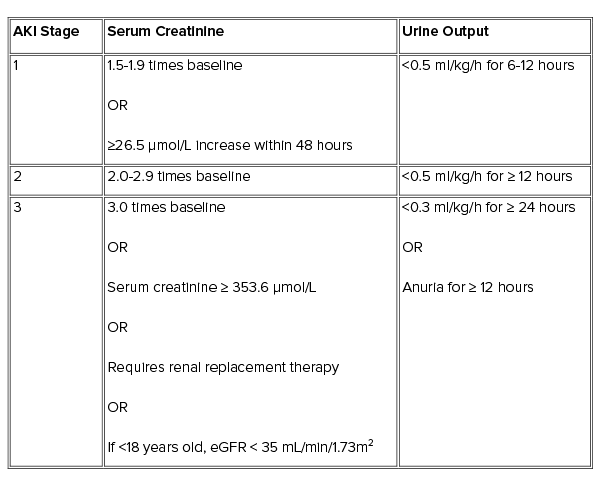
- AKI is diagnosed based on serum creatinine (SCr) levels or decreased urine output.
- eGFR is NOT applicable in AKI.
- AKI Staging criteria based on Kidney Disease: Improving Global Outcomes definitions.
- Baseline creatinine measurements may not be available. Patients at increased risk of AKI should have SCr and urine output monitored.
Clinical Evaluation
Try to determine the cause (prerenal, intrarenal, postrenal).
- Prerenal and postrenal causes are the most common and attempts should be made to rule these causes out prior to workup for intrarenal causes.
Prerenal
- Hemorrhage
- GI/urinary fluid loss
- Sepsis
- Postoperative hypotension
- ACEi/ARBs
- NSAIDs
Postrenal
- Prostate hypertrophy/cancer
- Kidney stones
- Neurogenic bladder
Intrarenal
- Nephritic syndrome
- Hematuria
- Proteinuria
- HTN
- Nephrotic syndrome
- HTN
- Periorbital swelling
- Lower leg edema
- Rhabdomyolysis
- Nephrotoxic agents
- Drug eruption
- Infections
Investigations
Investigations are guided based on the likely cause (prerenal, intrarenal, postrenal). Postrenal causes CANNOT be ruled out based on urine output.
Lab investigations:
- Serum creatinine
- BUN
- Electrolytes
- CBC
- CK
- ABG or VBG
- pH
- HCO3
- pCO2
- ECG:
- Hyperkalemia causing ECG changes
- Urinalysis:
- Dipstick
- Microscopy
- Albumin or Protein to Creatinine ratio
- Urine electrolytes
- Urine sodium concentration < 20 mmol/L indicates prerenal cause (3)
- Urine Osmolality
- Imaging:
- Ultrasound for postrenal obstruction and post-void volume
- CT for obstruction or unexplained cause of AKI
- Biopsy (consult nephrology)
Recommended Treatment
- Management of AKI is mostly supportive.
- Life-threatening complications may arise and need to be treated promptly.
- Early nephrology consultation may be beneficial.
Discontinue Nephrotoxic Agents
- Pharmacist review or use of a drug lookup database (e.g. Lexicomp, RxTx) may be beneficial.
- Examples:
- NSAIDs
- ACEi/ARB
- Aminoglycosides
- Adjust Medications for Renal Dosing
- Pharmacist review or use of a drug lookup database (e.g. Lexicomp, RxTx) may be beneficial.
- Volume Status
- Hypovolemia:
- Renal perfusion needs to be balanced with fluid overload.
- 9% normal saline or lactated Ringer’s solution are recommended over colloid solutions (1, 2). Plasmalyte can also be used.
- Target Mean Arterial Pressure >65 mmHg.
- Vasopressors may be used if fluid resuscitation is not successful (1, 2, 3).
- Hypervolemia:
- Furosemide:
- Initial: 80 mg IV or double the patient’s usual dose if already on diuretic (5).
- If no improvement in urine output within 2 hours, double initial dose (5).
- Renal Replacement Therapy (Indications below)
- Furosemide:
- Hyperkalemia
- With ECG changes:
- Calcium Gluconate 1 g IV, repeat as needed (3).
- Insulin 10 Units IV with dextrose 25-50 g IV (3).
- Salbutamol 10-20 mg nebulized (3).
- Renal Replacement Therapy (Indications below)
- With ECG changes:
- Hypovolemia:
Potassium-restricted diet (<2g/day).
Metabolic Acidosis
- Treat underlying cause.
- IV fluids:
- Target serum bicarbonate 20-22 mmol/L and pH >7.2 (5).
- 9% Normal Saline, plasmalyte or Lactated Ringer’s solution for acidosis due to reduced perfusion.
- 3% Sodium Bicarbonate in D5W (3×50 mmol/50 mL ampules in 1L D5W) (5, 6).
- May also decrease serum potassium.
- Monitor for volume overload.
- Renal Replacement Therapy preferred if hypervolemic (indications below).
- Urinary Obstruction
- Urethral catheterization
- Consider Urology consultation
- Glycemic Control
- Target glucose 6.1 – 8.3 mmol/L (2)
- Renal Replacement Therapy
- Requires Nephrology consultation
- Indications (1):
- Despite adequate IV fluid administration:
- Anuria (>6 hours) or severe oliguria (< 200mL in 12 hours)
- Hyperkalemia (>6.5 mmol/L) despite treatments as mentioned above
- Severe metabolic acidosis (pH <7.2)
- Dialyzable toxin/drug
- BUN > 30 mmol/L
- Uremic complications (Encephalopathy, neuropathy, pericarditis)
- Volume overload unresponsive to diuretics
- Despite adequate IV fluid administration:
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Recommendations based off Kidney Disease: Improving Global Outcomes clinical practice guideline.
Related Information
Reference List
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Mar 31, 2021
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.