Acute Radiation Emergency
Environmental Injuries / Exposures
First 5 Minutes
What is the role of an ED physician in a nuclear emergency?
- Step (1) Prepare the ED
- Initiate Code Orange procedures if applicable. Enact local nuclear safety plan if available.
- Establish decontamination zones, cordon off contaminated zones, secure entrances. Create a triage station external to ER. Ensure unidirectional flow through the ER. Deploy PPE, radiation monitoring equipment (Geiger counters), take baseline radiation level of ED.
- Don appropriate PPE for all staff. Utilise extra precautions in treating patients (e.g., extra bed sheets, disposable PPE, patient spacing).
- Involve psychological supports for patients & staff early on.
- Coordinate with local agencies – what resources are needed, scale of problem, prepare for mass patient transport, etc.
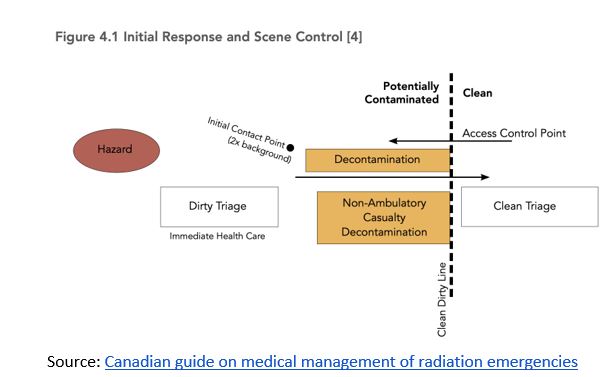
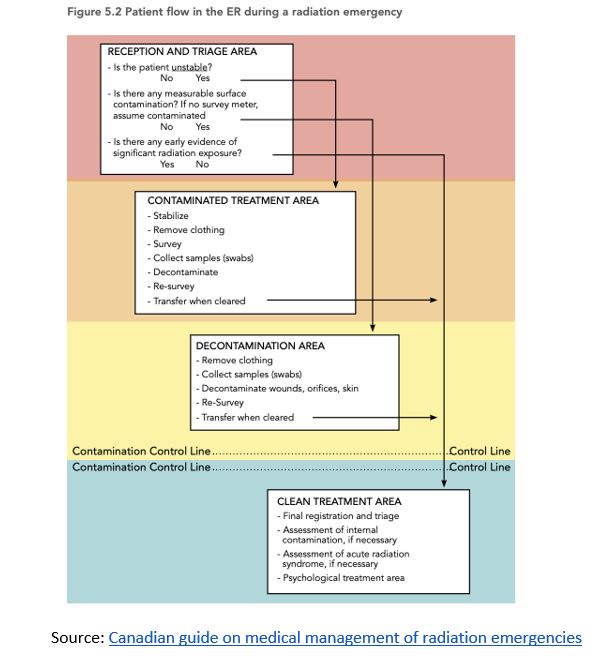
- Step (2) Decontaminate patients external to ER
- EXCEPTION: For patients with life-threatening injuries, treat first and decontaminate later.
- Assume all patients are contaminated unless prior decontaminated.
- Preliminary decontamination (remove clothes, wash patients full body). Document contaminated areas on body chart.
- For open wounds DO NOT scrub vigorously – irrigate gently.
- Survey, decontaminate face and its orifices.
- Skin and hair from highest to lowest radioactivity areas.
- Re-survey
- Vulnerable host factors (extreme ages, immunosuppressed, chronic disease, pregnant)Triaging specific to radiation injury.
- Higher radiation dose received = worse prognosis. Estimate dose using this calculator Estimator for Exposure.
Relevant resources:
Context
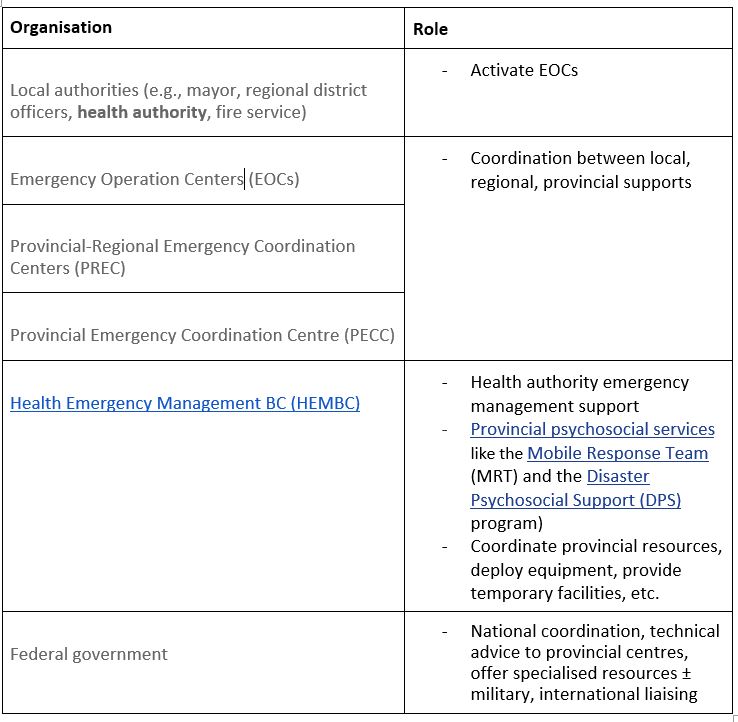
Who does what during a nuclear emergency?
In the rare event of nuclear emergency, federal and provincial plans exist which outline the roles of various authorities.
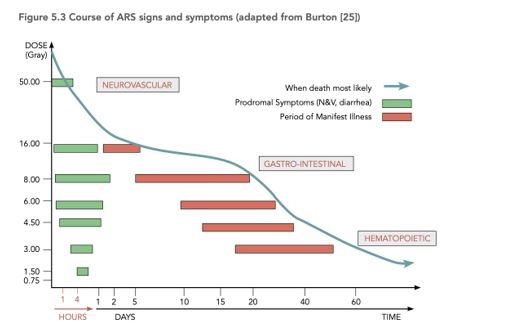
Severity of injury is dose dependent
It is critical to estimate dose received as dose predicts prognosis and tailors management.
- 1 Gy (minimum to get ARS)
- 5 Gy (kills 50% exposed)
- ≥10 Gy (kills 100% exposed)
https://publications.gc.ca/collections/collection_2017/sc-hc/H129-49-2015-eng.pdf
Diagnostic Process
Medical assessment and initial management
- History, Physical, Investigations
- Gather essential information to inform the management of ARS subsyndromes through Hx, PEx, investigations.
- Estimating dose received is essential in tailoring management and informing prognosis. Use this calculator which includes onset to vomiting and serial lymphocyte depletion metrics: Dose Estimator for Exposure: 3 Biodosimetry Tools.
- Hx
- Age
- Exposure history (distance from source, time exposed, any shielding?)
- PMHx that would increase risk (immunocompromised, currently pregnant, Fanconi anemia, MMR mutations).
- PEx & ROS
- Vitals
- Neurological – cognitive deficits, focal deficits
- Cutaneous – erythema, edema, desquamation, hair loss, abnormal sensation, blistering, ulcer/necrosis, onycholysis
- HEENT – headache
- GI – nausea, vomiting, diarrhoea, stool consistency, mucosal loss, abdo cramps/pain, GI bleeds
- Haematological – bleeding history
- Constitutional – anorexia, fatigue, nausea
- Initial labs
- CBC + differential (repeat every hour to measure lymphocyte depletion)
- Chemistries
- Baseline INR/PTT, type and screen
- Urinalysis
- Special labs
- 24h post exposure blood draw into lithium heparin tube → send to lab for chromosome aberration testing.
- HLA typing (preparation for bone marrow transplant).
-
- Imaging
- XR, CT for internal organ damage.
- Imaging
Relevant Resources:
Adult Medical Orders for Radiation Injury Treatment
Pediatric Medical Orders for Radiation Injury Treatment
- Recognize Acute Radiation Syndrome (ARS)
- ARS occurs after exposure to high-dose, penetrating radiation exposure to most or all of the body.
- ARS physical signs are non-specific:
https://www.env.go.jp/en/chemi/rhm/basic-info/2018/03-03-02.html
-
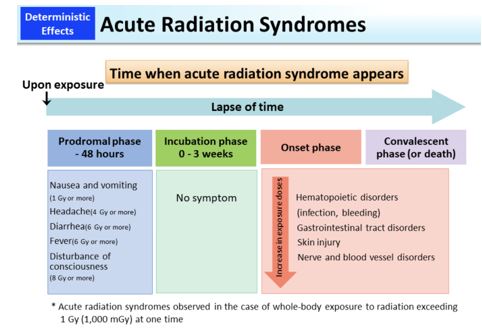
- ARS natural history: radiation exposure → hours/days/weeks can elapse → non-specific clinical features (often n/v, h/a, diarrhea).
- Phases of ARS:
- Prodromal (0-2d post exposure): anorexia, n/v, fatigue, tachy, fever, h/a.
- Latent (2-20d post exposure): Few or absent s/s. Duration inversely proportional to dose received.
- Manifest (21-60d post exposure): Natural history = Infection, anaemia, bleeding → severe diarrhoea, hypovolemia, lytes disturbances → altered mental status, cerebral edema, CV collapse.
- Recovery: Prognosis and duration dose-dependent.
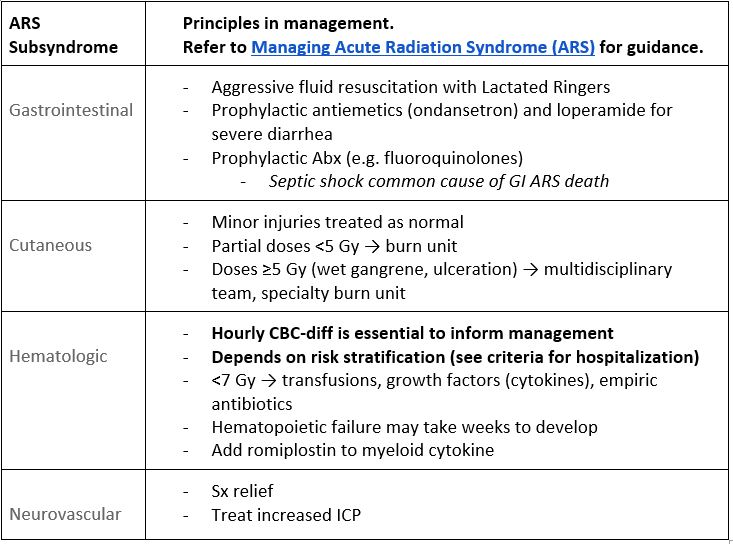
- Four subsyndromes: (1) Hematopoietic, (2) Gastrointestinal, (3) Cutaneous, and (4) Neurovascular.
- Consult refer early on
- Involve multidisciplinary team approach to manage complications (surgery, internal medicine, intensive care, transplant medicine, etc.)
- Communicate with authorities
- Communication with local/regional authorities as laid out in BC Nuclear Safety Plan (2020) .
Recommended Treatment
Principles of treatment
- Prioritise treating life-threatening injuries over decontamination.
- Multidisciplinary management for radiation and non-radiation inflicted injuries (e.g., surgeon, burn team, dermatology, GI docs, neuro, haematologists).
- Use added precautions in treating contaminated patients (e.g. extra bed sheets, diligently dispose of PPE and label “contaminated”).
- Admit all patients with ARS and refer to appropriate specialists. Prepare for transport to specialised centres where indicated.
Treat by subsyndrome
Criteria For Hospital Admission
Hospital admission
- Due to risk of hematopoietic injury, hospitalize all patients with
- injuries from radiation (e.g. trauma, burns);
- age ≤12y or ≥60y; or
- Any patients with estimated dose received ≥3 Gy (calculator for Estimator for Exposure).
Criteria For Transfer To Another Facility
Transfer decisions based on availability of services at current center and predicted patient needs (e.g., ICU, bone marrow transplant).
Criteria For Close Observation And/or Consult
Consults and follow-up
- Seek ongoing assessment days to weeks post exposure.
- ARS usually resolves in 2 months. Prognosis is poor.
- Long-term follow-up with primary care (e.g. cancer surveillance) is warranted.
- Psychological trauma – talk to doctor, counsellors about symptoms of anxiety, depression, PTSD.
- Children should have thyroids checked regularly.
- Regular eye exams for cataract development in patients exposed to neutrons.
Relevant resource: Follow-up Instructions for Individuals Involved in a Radiological or Nuclear Emergencies
Criteria For Safe Discharge Home
- No other toxicity, adverse features, stable.
- Estimated ≤3 Gy.
- Pose no contamination risk to others.
- Refer to Follow-up Instructions for Individuals Involved in a Radiological or Nuclear Emergencies.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Limited real-life data on medical and situational management following nuclear disasters in modern times in Canada.
Related Information
OTHER RELEVANT INFORMATION
Comprehensive
- HIGH YIELD – Radiation Injury Treatment Network – Adult & Pediatric Treatment
- HIGH YIELD – US Department of Health & Safety Radiation Emergency Medical Management (REMM)
Quick Reference
- HIGH YIELD – REAC/TS Fact Sheet for Medical Providers
- HIGH YIELD – Dose Estimator for Exposure: 3 Biodosimetry Tools – Radiation Emergency Medical Management
- Hospital Orders Template – Adult
- Hospital Orders Template – Pediatric
- Checklist for Healthcare Personnel
- How to Perform a Survey for Radiation Contamination
- Body Chart for Recording Results of Radiation Survey
- How to Detect Radiation – ORISE
- Follow-up Instructions for Individuals Involved in a Radiological or Nuclear Emergencies
Apps
BC Specific
Canada Specific
- Canadian guide on medical management of radiation emergencies
- Interactive Tool to Determine Triage Category and Myeloid Cytokine Use after a Nuclear Detonation
Procedural Video: BEHR 2024 BEHRthoven Trueview EN 15sec (youtube.com)
Reference List
Dainiak N. Clinical manifestations, evaluation, and diagnosis of acute radiation exposure [Internet]. Danzl D, Chao N, Rosmarin A, Ganetsky M, editors. UpToDate. 2024 [cited 2024 Mar 7]. Available from: https://www.uptodate.com/contents/clinical-manifestations-evaluation-and-diagnosis-of-acute-radiation-exposure?search=acute%20radiation&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#references
Wingard J, Dainiak N. Management of radiation injury [Internet]. Danzl D, Chao N, Ganetsky M, Rosmarin A, editors. UpToDate. 2023 [cited 2024 Mar 7]. Available from: https://www.uptodate.com/contents/management-of-radiation-injury?search=acute%20radiation&topicRef=6589&source=see_link#topicContent
REMM – Radiation Emergency Medical Management [Internet]. remm.hhs.gov. Available from: https://remm.hhs.gov/
Disaster Psychosocial Support [Internet]. www.phsa.ca. [cited 2024 Apr 11]. Available from: http://www.phsa.ca/our-services/programs-services/health-emergency-management-bc/provincial-psychosocial-services/disaster-psychosocial-support
BC Nuclear Emergency Plan [Internet]. BC Provincial Emergency Plans. [cited 2024 Mar 7]. Available from: https://www2.gov.bc.ca/assets/gov/public-safety-and-emergency-services/emergency-preparedness-response-recovery/embc/plans/bc_nuclear_emergency_plan.pdf
Canada H. Canadian Guide on Medical Management of Radiation Emergencies [Internet]. www.canada.ca. 2014 [cited 2024 Mar 7]. Available from: https://publications.gc.ca/collections/collection_2017/sc-hc/H129-49-2015-eng.pdf
Radiation Emergency Assistance Center/Training Site (REAC/TS) [Internet]. Oak Ridge Institute for Science and Education. Available from: https://orise.orau.gov/reacts/
Dainiak N, Gent RN, Carr Z, Schneider R, Bader J, Buglova E, Chao N, Coleman CN, Ganser A, Gorin C, Hauer-Jensen M. Literature review and global consensus on management of acute radiation syndrome affecting nonhematopoietic organ systems. Disaster medicine and public health preparedness. 2011 Oct;5(3):183-201.
Dainiak N, Gent RN, Carr Z, Schneider R, Bader J, Buglova E, Chao N, Coleman CN, Ganser A, Gorin C, Hauer-Jensen M. First global consensus for evidence-based management of the hematopoietic syndrome resulting from exposure to ionizing radiation. Disaster medicine and public health preparedness. 2011 Oct;5(3):202-12.
RITN Acute Radiation Syndrome Treatment Guidelines [Internet]. Radiation Injury Treatment Network. 2020 October. [cited 2024 Mar 7]. Available from https://ritn.net/treatment
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Apr 11, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.