Acute Transfusion Reaction
Critical Care / Resuscitation, Hematological / Oncological
First 5 Minutes
- If a transfusion reaction is suspected, stop the transfusion, assess ABCs, and maintain IV access.
Context
- Acute transfusion reactions can broadly be classified into immune and non-immune reactions.
- Acute transfusion reactions can range from mild fever and/or pruritis to life threatening shock and Disseminated Intravascular Coagulation (DIC).
- Types of Acute Transfusion Reactions:
- Transfusion Associated Circulatory Overload (TACO)
- Relatively common, less than 1% of transfusions, though may be underreported
- Potentially life threatening.
- Higher risk in patients with pre-existing volume overload, due to conditions such as kidney disease, or heart failure.
- Results in acute respiratory distress, secondary to cardiogenic pulmonary edema.
- Transfusion Associated Lung Injury (TRALI)
- Historically, highest mortality rate (overtaken by TACO in 2016).
- Respiratory distress, secondary to non-cardiogenic pulmonary edema.
- Etiology is the activation of leukocytes within pulmonary vasculature, following transfusion of a product with anti-HLA, or anti-neutrophil antibodies.
- Acute hemolytic transfusion reaction (AHTR)
- Rare, mortality rate from 8-44%.
- Iatrogenic: transfusing incompatible blood.
- Hemolysis secondary to ABO-incompatibility, and incompatibility with other blood components.
- Complications can include DIC, and AKI.
- Transfusion Associated Sepsis
- Bacterial contamination is rare.
- The risk is higher in platelet transfusions.
- Anaphylactic transfusion reaction
- Rare, approximately 1 in 50, 000 transfusions.
- Allergic transfusion reaction
- Relatively common, and self-limiting.
- May be reacting to plasma proteins in donor blood.
- Febrile non-hemolytic reaction (FNHTR)
- Most common,4 of 1000 transfusions in Canada.
- Etiology believed to be inflammatory cytokines, or antibodies against donor leukocytes.
- Diagnosis of exclusion.
- Transfusion Associated Circulatory Overload (TACO)
Diagnostic Process
- Diagnosis is clinical.
- Investigations can determine the specific etiology, however the initial management should be based on the clinical presentation.
- Treatment should not be delayed in order to complete investigations.
- Fever, chills, pruritis, and urticaria may indicate a mild reaction, and self resolve.
- Signs and symptoms such as altered level of consciousness, hypotension, respiratory distress, hypertension, tachycardia, flank pain, oozing from IV, oliguria, and anuria suggest a life-threatening reaction.
- Presentation types:
- Dyspnea
- Consider TACO, TRALI, or anaphylaxis.
- Investigations
- CBC, liver enzymes, electrolytes, creatinine, +/- BNP.
- CXR.
- Fever
-
- TRALI, sepsis, AHTR, or FNHTR.
- Confirm correct product transfused.
- Presentation unlikely to be secondary to contamination if fever is mild, spontaneously resolves, and lacks associated systemic signs and symptoms.
- Investigations
- CBC, liver enzymes, electrolytes, creatinine.
- Direct Antibody Test, LDH, haptoglobin, bilirubin.
- Repeat crossmatch.
- Urinalysis.
- PT, aPTT, fibrinogen.
- Blood cultures from patient, and donor blood products.
- Gram stain.
-
- Hypotension
- TRALI, AHTR, and sepsis.
- Investigations
- Same as fever.
- Dyspnea
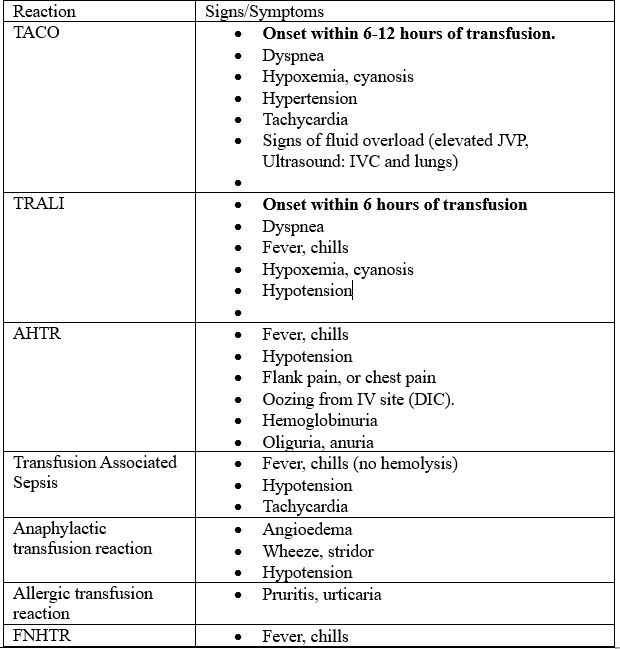
Clinical Presentations of specific acute transfusion reactions
Recommended Treatment
- Stop the transfusion, and ensure the patient is clinically stable.
- Confirm details of the product that was transfused, and report to transfusion services.
- Evaluate for specific signs and symptoms to determine specific etiology (discussed above).
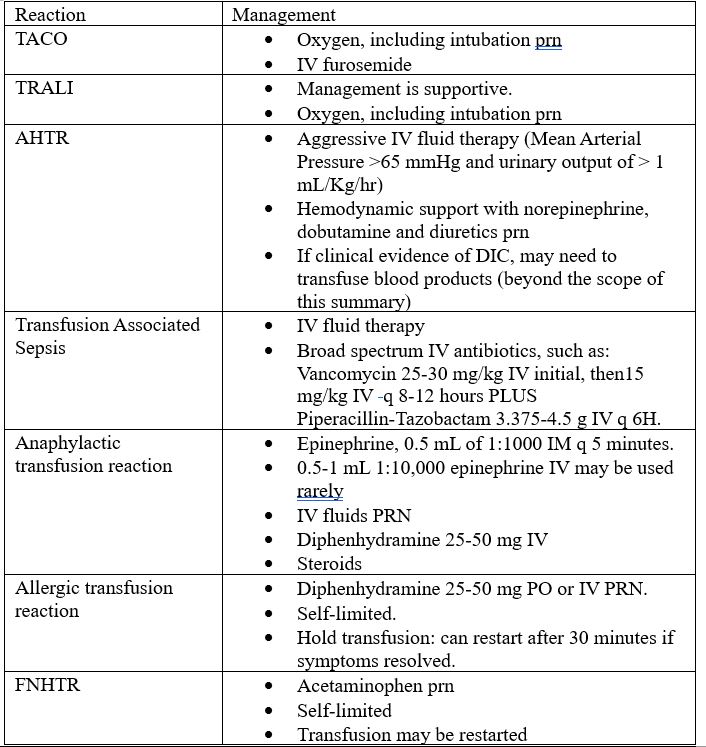
Definitive management for specific transfusion reactions.
Criteria For Hospital Admission
- Patients with life threatening transfusion reactions require admission.
Criteria For Transfer To Another Facility
- Patients with life threating reactions require transport to a center with ICU capability.
Criteria For Close Observation And/or Consult
- In patients with confirmed AHTR, nephrology and hematology (or transfusion medicine) consults may be appropriate.
- TRALI, and TACO, may warrant ICU, cardiology, respirology consults, and admission.
Criteria For Safe Discharge Home
- Patients with mild, non-life-threatening transfusion reactions are appropriate for discharge, if the reaction resolves.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
General approach is consistent amongst sources, though most information is based on society recommendations. There is some disagreement as to specific definitions amongst differing sources.
Related Information
OTHER RELEVANT INFORMATION
Allergic Reaction: https://www.bcemergencynetwork.ca/wp-content/uploads/2019/12/Allergic-Reaction-1.pdf
Emergency Medicine Cases, Episode 36: Transfusions, Anticoagulants and Bleeding (Podcast)
Reference List
Carson JL, Triulzi DJ, Ness PM. Indications for and Adverse Effects of Red-Cell Transfusion. Longo DL, editor. N Engl J Med. 2017 Sep 28;377(13):1261–72.
Frazier SK, Higgins J, Bugajski A, Jones AR, Brown MR. Adverse Reactions to Transfusion of Blood Products and Best Practices for Prevention. Critical Care Nursing Clinics of North America. 2017 Sep;29(3):271–90.
Laureano M, Khandelwal A, Yan M. [Internet]. TRANSFUSION REACTIONS. Clinical guide to transfusion. Ottawa: Canadian Blood Services, 2022.
Soutar R, McSporran W, Tomlinson T, Booth C, Grey S. Guideline on the investigation and management of acute transfusion reactions. Br J Haematol. 2023 Jun;201(5):832–44.
Tobian A, Steven Kleinman, Jennifer S. Tirnauer. UpToDate. [cited 2023 Jul 18]. Approach to the patient with a suspected acute transfusion reaction – UpToDate. Available from: https://www.uptodate.com/contents/approach-to-the-patient-with-a-suspected-acute-transfusion-reaction?search=acute%20transfusion%20reaction&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Dec 24, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.