Asthma Exacerbation in Adults – Treatment
Inflammatory, Respiratory
Context
- 8% of Canadians > 18 years have asthma.
- Onset is less common with increasing age.
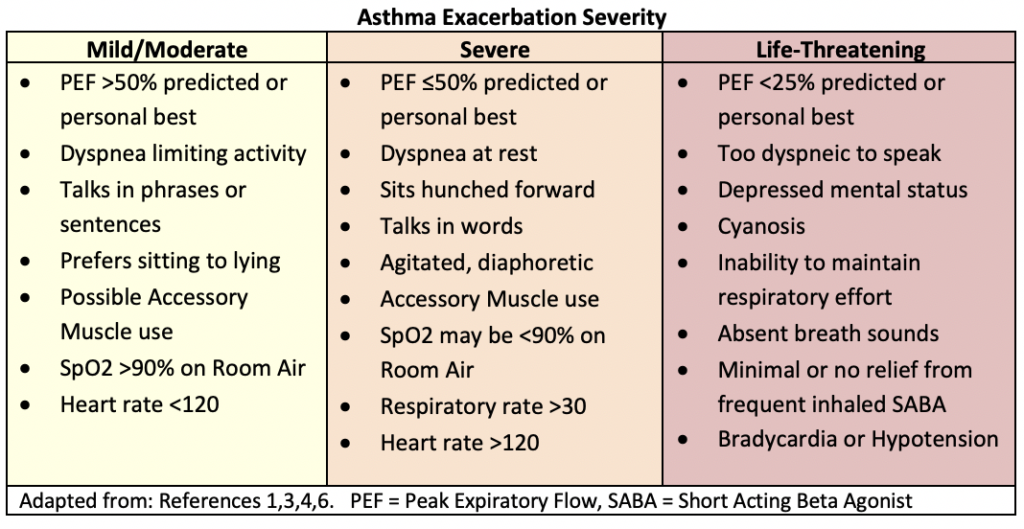
- Typically presents with dyspnea, cough, wheezing and chest tightness.
- Severe cases can be fatal.
Recommended Treatment
Standard Treatment
- Oxygen
- Maintain O2 Saturations >92%.
- Usually not necessary for mild or moderate exacerbations.
- Short Acting Beta Agonist (SABA)
- Metered Dose Inhaler (MDI) Salbutamol (100 mcg/puff) with spacer.
- 4 to 8 puffs q20 minutes x 3 doses, then every 1 to 4 hours prn.
- Nebulized Salbutamol 5-5mg in 3 mLs saline q20 minutes x 3 doses, then 2.5-10mg every 1 to 4 hours prn.
- If severe exacerbation – give more frequently or continuous.
- Metered Dose Inhaler (MDI) Salbutamol (100 mcg/puff) with spacer.
- Anticholinergics
- Use alongside SABA for moderate or severe exacerbations.
- MDI Ipratropium bromide (20mcg/puff) with spacer.
- 4 to 8 puffs q 20 minutes x 3 doses, then prn.
- Nebulized Ipratropium bromide 500mcg (with salbutamol) q20 minutes x 3 doses, then q2-6 prn.
- If severe exacerbation – give more frequently or continuous.
- Glucocorticoids
- Oral prednisone 50mg OR equivalent.
- If oral not possible – IV methylprednisolone 40-125mg.
- May not be necessary for mild exacerbation (depending on patient’s history).
- Magnesium Sulphate
- For severe exacerbations not responding to initial therapies.
- 2g Magnesium Sulphate in 100mL D5W given intravenously over 20mins.
Worsening Severe or Life-threatening Exacerbation
Complete Standard Treatment and consider the following:
- Specialist consult.
- Consider alternate diagnosis: anaphylaxis, pneumothorax, airway obstruction.
- Portable CXR and ABG.
- Non-Invasive Ventilation or Intubation.
- Adjunctive treatments.
Consider Non-Invasive Ventilation (NIV) in patients not responding to medical therapy if intubation is not imminently required.
- Indicators:
- Tachypnea RR >25/min.
- Tachycardia 110/min.
- Use of accessory muscles of respiration.
- Hypoxia with a PaO2/ FiO2 ratio, or P/F ratio <200.
- Hypercapnia with PaCO2 <60 mmHg.
- FEV1 <50% predicted.
- Avoid NIV if:
- Agitation or decreased level of consciousness (LOC).
- Vomiting or profuse secretions.
- Significant haemodynamic instability.
Intubation if NIV is unsuitable or ineffective
- Maximize medical treatment prior to intubation if possible.
- Indications:
- Decreased LOC.
- Respiratory fatigue/silent chest.
- Inability to maintain oxygenation with non-invasive methods.
- Worsening hypercapnia or severe acidemia (pH < 7.10).
- Hemodynamic instability.
Consider Adjunctive Treatments
- Ketamine:
- May relieve bronchospasm and help avoid intubation.
- Limited experience, ideal dosing not determined.
- Bolus 0.1 mg/kg to 2 mg/kg. (Note: 1-2 mg/kg = dose for intubation)
- Continuous infusion 0.15 – 2.5 mg/kg/hr, if good response to bolus.
- Salbutamol by IV infusion:
- IV bolus 4mcg/kg then continuous infusion 0.1-0.2 mcg/kg/min.
- Epinephrine:
- IM 0.3-0.5mg q20mins prn.
- IV 0.1mg over 5-10mins and q5-15mins prn, OR IV Infusion 1-4mcg/min.
- Heliox:
- 70:30 (He:O2) – Reduces turbulent air flow to improve ventilation.
- General Inhalational Anesthesia:
- Potent bronchodilators, but evidence is limited – consult anesthesia.
- Halothane, isoflurane, sevoflurane, desflurane.
Criteria For Hospital Admission
- Patients with non-life-threatening exacerbations who improve, but do not meet discharge criteria, can undergo a trial of observation before admission.
Criteria For Transfer To Another Facility
- Transfer to an acute care center for mild or moderate exacerbations worsening despite treatment, or for any severe or life-threatening exacerbation.
Criteria For Close Observation And/or Consult
- Consider ICU consult for life-threatening exacerbations or severe exacerbations which do not improve.
Criteria For Safe Discharge Home
Criteria for discharge must be individualized but in general include:
- Asymptomatic or substantially improved symptoms.
- Peak Expiratory Flow (PEF) >80% or PEF 60-80% and improving.
- Normal oxygen saturation.
- No history of near-death exacerbations.
- Understanding of asthma management, and ability to return if worsening.
Arrange at discharge:
- Reliever and Controller Medications.
- Inhaler technique, importance of adherence and action plan.
- 50mg Prednisone PO (OR equivalent) daily for at least 5 days.
- Instructions for follow up with primary care at end of 5 days (based on steroid duration).
- Instructions on returning if worsening dyspnea (PEF < 200 L/min or use of inhaler <2h interval), chest pain, confusion or weakness.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Evidence comes from sources published within the last few years, including the 2019 GINA guidelines, which are in relative agreement on asthma exacerbation management.
Quality of evidence is low for life-threatening exacerbation management.
Related Information
Reference List
Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2019.
Lung Health Foundation: Adult Emergency Department Asthma Care Pathway (EDACP), June 2018.
Sourav Majumdar. Acute asthma exacerbation in adults. BMJ Best Practice. June 2018
-
-
-
Asthma, by age group. Statistics Canada. Table 13-10-0096-08.
-
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Aug 25, 2020
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.