Bronchiolitis in Infants and Toddlers (and differentiating this from Asthma)
Cardinal Presentations / Presenting Problems, Infections, Pediatrics, Respiratory
Context
- Bronchiolitis Definition: First episode of wheezing in infants <12 months age.
- Acute infectious syndrome in infants caused by viral LRTI.
- Characterized by inflammation, edema and necrosis of epithelial cells lining small airways, the result of which is increased mucus production.
- Symptoms: rhinitis, cough, tachypnea, accessory muscle use, wheeze, crackles. As mucous can move within airways, signs/symptoms are known to vary within minutes to hours.
- Most common pathogen: Respiratory Syncitial Virus (RSV) >> Human Rhinovirus > other viruses.
- Occurs typically: December to March in North America.
- In the first year of life:
- 90% of infants infected with RSV.
- 20% seek outpatient medical attention for bronchiolitis.
- 2% – 3% are hospitalized (even fewer require critical care).
Diagnostic Process
- Is there a recommended decision aid?
-
- No clinically validated decision aid yet exists.
- If so, what is it and how do you use it?
- N/A
- If no decision aid, what investigative process do you recommend?
- Bronchiolitis is a clinical diagnosis. No workup is advised.
- Important limitations or pitfalls of testing/interpretation of test results.
- The vast majority of patients presenting with bronchiolitis will have mild/moderate disease severity.
- Children with risk factors for severe disease (immunodeficiency, history of premature birth <32 weeks GA, age <48 weeks post conception, underlying cardiopulmonary disease) or those who are very unwell (RR >70, oxygen saturation <90% on room air, marked work of breathing, lethargy) deserve investigation and a trial of treatment.
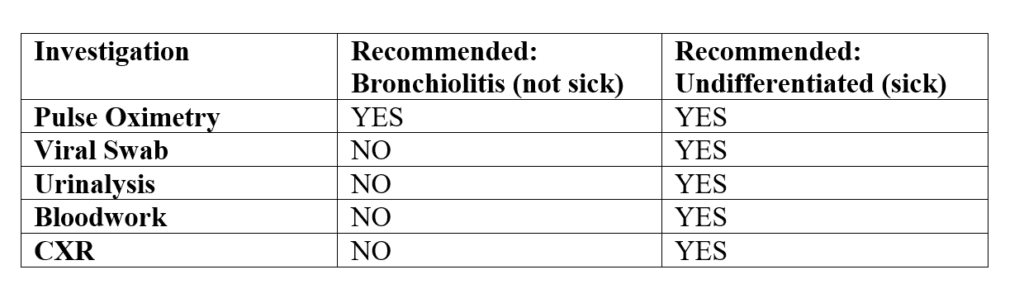
- Table summarizing recommended investigations for bronchiolitis, per 2014 Bronchiolitis Clinical Practice Guideline. Note: Column 3 is supported by expert opinion, rather than by evidence, but is reasonable for the small subset of children presenting with severe illness.
-
How to differentiate bronchiolitis from asthma?
-
- ≥2 wheezing episodes occurring <1 year of age should raise the suspicion of asthma and prompt consideration of a referral to a specialist for evaluation.
- The best way to distinguish bronchiolitis from asthma in the ED, is probably by the response to a trial of salbutamol metered-dose inhaler.
- How to do a trial of salbutamol MDI:
- Calculate PRAM score.
- Administer salbutamol via MDI with aerochamber, according to Provincial ED Asthma algorithm.
- Assess for clinical response in 15 minutes.
- If demonstrated improvement in oxygen saturation, work of breathing, the patient should be diagnosed with ASTHMA.
- Note: a patient can suffer from bronchiolitis and asthma simultaneously.
- Terms such as bronchospasm, reactive airways disease, wheezy bronchitis and happy wheezer should be abandoned.
Nuance:
-
- Airways in children:
- <6 months old lack B-agonist receptors, so salbutamol should never be trialed.
- >9 months old have developed B-agonist receptors, so salbutamol should be trialed.
- Between 6-9 months of age, it is reasonable to perform a trial of bronchodilators in a patient with risk factors for asthma.
- Airways in children:
Recommended Treatment
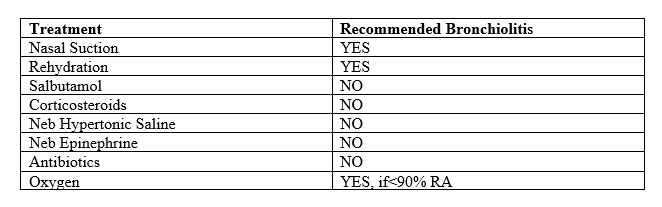
Table summarizing recommended treatments for bronchiolitis, per 2014 Bronchiolitis Clinical Practice Guideline. Antipyretics + nasal suction + oral/NG tube rehydration are often sufficient treatment.
Criteria For Hospital Admission
- Oxygen saturation <90% awake or asleep.
- Inadequate feeding / hydration.
- Marked work of breathing / lethargy.
- Caregiver not able to care for child at home / not able to return to ED for reassessment.
Criteria For Transfer To Another Facility
Oxygen saturation <90% despite 2 L/kg/min of 100% oxygen via nasal cannula.
Criteria For Close Observation And/or Consult
Refer to criteria for hospital admission.
Criteria For Safe Discharge Home
- Oxygen saturation >90% room air, awake and asleep.
- Adequate feeding / hydration.
- Mild/moderate work of breathing.
- Caregiver able to monitor symptoms and return for reassessment if concerned about deterioration.
- Discharge instructions and considerations:
- Acetaminophen 15 mg/kg q6h + ibuprofen 10 mg/kg q6-8h.
- Nasal suction.
- Monitor feeding / hydration.
- Return to ED if fever >5 days, inadequate feeding / hydration, lethargy.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Investigation and treatment of bronchiolitis.
Bronchiolitis severity assessment.
Related Information
OTHER RELEVANT INFORMATION
Patient Discharge Sheet https://www.albertahealthservices.ca/assets/heal/heal-handout-cough-wheeze.pdf
Reference List
Clinical Practice Guideline: The Diagnosis, Management, and Prevention of Bronchiolitis. pediatrics.org/cgi/doi/10.1542/peds.2014-2742. doi:10.1542/peds.2014-2742.
Diagnosis and management of asthma in preschoolers: A Canadian Thoracic Society and Canadian Paediatric Society Position Paper. Paediatric Child Health Vol 20 No 7 October 2015.
Cody Meissner, M.D. Viral Bronchiolitis in Children. N Engl J Med 2016;374:62-72.DOI: 10.1056/NEJMra1413456.
Diagnosis and Management of Bronchiolitis Subcommittee on Diagnosis and Management of Bronchiolitis. PEDIATRICS Volume 118, Number 4, October 2006.
BCGuidelines.ca: Asthma in Children – Diagnosis and Management (2015).
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Oct 06, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.