Carbon Monoxide Toxicity: Diagnosis
Environmental Injuries / Exposures, Neurological, Toxicology
Context
- Carbon Monoxide (CO) is a colourless, odourless, tasteless gas formed from the incomplete combustion of hydrocarbons.
- Sources include: house fires, heating systems, charcoal grills, and motor vehicles, especially in areas with poor ventilation.
- Most common acute presentations are after intentional self-exposure or entrapment in a house fire. Chronic presentations due to ongoing household exposure are less common.
- Every year, the Vancouver General Hospital Hyperbaric Unit treats around 40 cases of CO poisonings, and there are approximately 300 CO related deaths in Canada. CO Toxicity is the most common cause of fire-related death.
- CO strongly binds to hemoglobin forming carboxyhemoglobin (COHb), which reduces oxygen carrying and delivering capacity leading to tissue hypoxia. It also binds to cytochromes directly, causing direct cellular damage, and initiates an inflammatory cascade that includes lipid peroxidation leading to both immediate and delayed neurologic damage.
- Diagnosis can be difficult, as chronic exposures can present with vague or nonspecific symptoms and patients may not be aware of their exposure history.
Diagnostic Process
- Ask about possible exposure sources, and household members with similar symptoms.
- Symptoms and Signs include:
- Nonspecific: headache, nausea/vomiting, fatigue, “flu-like” symptoms. The classic “Cherry Red” lips and skin are rarely seen in the ED, as they are correlated with lethal COHb levels, and are most often seen in the morgue.
- Cardiovascular: dyspnea, chest pain, dysrhythmias, hyper or hypotension
- CNS: confusion, altered level of consciousness, focal neurologic signs, seizures, coma. In subtle cases, a detailed neurologic exam should be done looking for subtle findings, which may determine whether patients require hyperbaric treatment. Loss of consciousness is a major risk factor for developing delayed neurologic sequelae.
- Delayed Neurologic Sequelae: up to 4 weeks after exposure, neurologic or psychiatric symptoms including cerebellar abnormalities, parkinsonism, and memory deficits.
- CO may be diffused from the blood within hours of removal from the exposure, especially if started on high flow oxygen (t1/2 = 5 hours on room air, 1 hour on 100% FiO2), so early testing is key to a confirmed diagnosis. Standard of care is an ABG with co-oximetry to measure %COHb.
- In the field, fingertip pulse co-oximetry may be used to raise suspicion, but may be inaccurate; ACEP 2017 guidelines recommended against using them.
- In hemodynamically stable patients, venous samples are just as accurate for COHb levels, and are commonly used.
- Elevated COHb = >4% in non-smokers, >10% in smokers. For each pack of cigarettes smoked per day, the COHb rises about 2.5%.
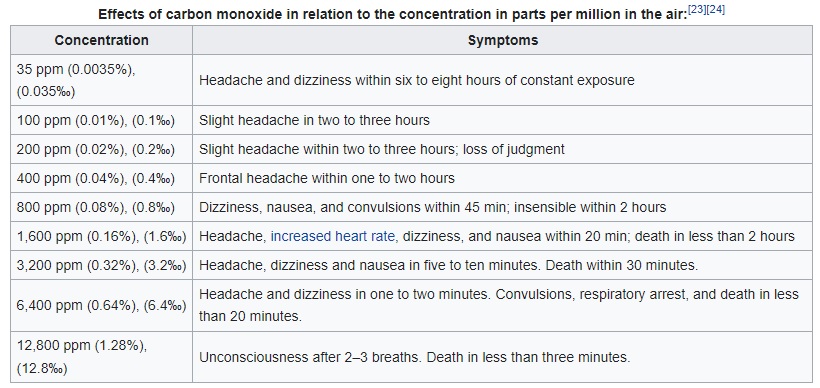
- These levels are important both to establish diagnosis, and may change the decision to initiate hyperbaric treatment, but there is no validated relationship between COHb level and symptom severity.
- ABG may also show elevated lactate, and metabolic acidosis.
- Further workup may include:
- EKG: for dysrhythmias or ischemic changes.
- Troponin: for myocardial damage.
- bHCG in all women of childbearing age.
- CT Head to rule out other causes of neurologic decompensation.
- If intentional self-exposure, consider co-intoxicants.
- If a house or industrial fire, include Cyanide level.
- Remember that normal SpO2 can NOT exclude CO exposure – most pulse oximeters cannot differentiate carboxyhemoglobin from oxyhemoglobin, so SpO2 may read 100% with good wave form in a patient who is critically hypoxic from CO toxicity.
- Remember that PO2 measurements tend to be normal or high, as they reflect O2 dissolved in blood only, which is not affected by CO. A patient may have a normal PO2 but still be critically hypoxic.
- CO Toxicity is a clinical diagnosis, which requires the following:
- History of potential CO exposure.
- Symptoms consistent with CO toxicity.
- Elevated carboxyhemoglobin level – although given the time-sensitive nature of this test, a normal COHb cannot always rule out the diagnosis.
Once diagnosis is established, patient signs and symptoms guide management, not levels – so repeat measurements are generally unnecessary.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Moderate to high quality evidence re. diagnosis and epidemiology have emerged in the last 2 decades. Low quality evidence leading to ongoing uncertainty in diagnosis and treatment of long term neurologic sequelae.
Related Information
Reference List
Weaver LK. Carbon Monoxide Poisoning. New England Journal of Medicine. 2009;360(12):1217-1225.
-
Thomas A, Lipp C. Chapter 159. Inhaled Toxins. March 2019.
Cohen I, Garis L, Rajabali F, Pike I. Carbon Monoxide Poisoning. BC Injury research and prevention unit. October 2017:1-21.
Relevant Resources
RELEVANT RESEARCH IN BC
System Response to Toxicologic EmergenciesRESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Oct 27, 2020
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.