Dental Facial Nerve Blocks
Ears, Eyes, Nose, and Throat, Other
Context
Superficial Face
Overview
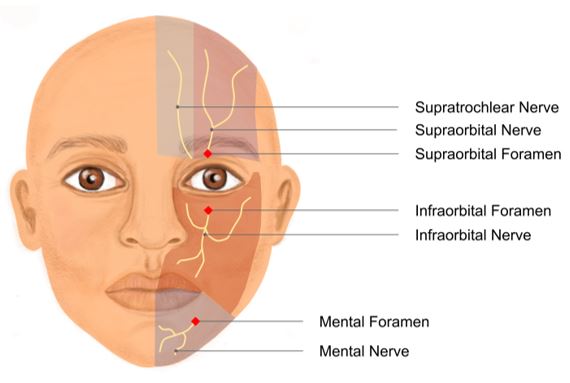
- Sensory innervation of the face is predominantly mediated by the supratrochlear, supraorbital, infraorbital and mental nerves.
Supratrochlear / Supraorbital
Injection Site | Supraorbital foramen
Equipment | 3-10 ml syringe, 25 or 27 GA needle
Anesthetic | 1-3 ml, Lidocaine 2% w/ Epi OR Bupivacaine 0.5%
Indications | Laceration repair and excisions of the lower forehead and upper eyelid
Contraindications | Inability to locate anatomical landmarks, pre-existing infection at site of injection, allergy to local anesthetic, lack of patient consent or cooperability
Anatomy
- Supraorbital nerve exits via supraorbital foramen
- Foramen located along the orbital rim, approximately at the junction of the medial 1/3 and lateral 2/3
- Most often found just medial to the pupil in the sagittal plane
- Supratrochlear nerve passes medially to the supraorbital foramen
Technique
- Palpate the supraorbital region for the supraorbital foramen.
- Insert the needle superficially and slightly inferior to the supraorbital foramen.
- Advance the needle ~5 mm medially and cephalad. Do not penetrate the supraorbital foramen.
- Aspirate to ensure no vascular entry.
- Slowly administer 1-3 ml of anesthetic over 30-60 seconds.
- For a supratrochlear block, partially retract the needle and re-angle ~1cm towards the midline.
- Administer an additional 0.5 ml of anesthetic.
- Massage the supraorbital foramen for ~10 seconds.
Infraorbital
Injection Site | Infraorbital foramen
Equipment | 3-10 ml syringe, 25 or 27 GA needle
Anesthetic | 1-3 ml, Lidocaine 2% w/ Epi OR Bupivacaine 0.5%
Indications | Laceration repair and excisions of the midface
Contraindications | Inability to locate anatomical landmarks, pre-existing infection at site of injection, allergy to local anesthetic, lack of patient consent or cooperability
Anatomy
- Infraorbital nerve exits medially and inferiorly from the maxillary bone via infraorbital foramen
- Foramen located in the midface, ~1cm inferior to the infraorbital rim
- Most often found just medial to the pupil in the sagittal plane
Technique (Percutaneous)
- Palpate the midface region for the infraorbital foramen.
- Insert the needle superficially and just inferior to the infraorbital foramen.
- Advance the needle medially and cephalad until the superior aspect of the foramen is met or paresthesia occurs. Do not penetrate the infraorbital foramen.
- If paresthesia occurs, withdraw the needle 1-2mm.
- Aspirate to ensure no vascular entry.
- Slowly administer 1-3 ml of anesthetic over 30-60 seconds.
Mental
Injection Site | Buccal mucosa between first/second premolars
Equipment | 3-10 ml syringe, 25 or 27 GA needle
Anesthetic | 1-3 ml, Lidocaine 2% w/ Epi OR Bupivacaine 0.5%
Indications | Laceration repair and excision of anterior lip/chin, buccal mucosa anterior to mental foramen
Contraindications | Inability to locate anatomical landmarks, pre-existing infection at site of injection, allergy to local anesthetic, lack of patient consent or cooperability
Considerations
- Mental nerve block may be useful when anesthesia of the anterior lip/chin is required but the teeth, tongue and mandible can be spared. Consider this nerve block instead of the inferior alveolar nerve block in these situations.
Anatomy
- Mental nerve is a terminal branch of the inferior alveolar nerve.
- Nerve exits the mental foramen on the anterior aspect of the mandible, approximately in line with the first or second premolars.
- Branches of the nerve run towards the midline and usually offer some degree of crossover innervation on the contralateral side.
Technique (Intraoral)
- Retract the patient’s lip laterally so that the buccal mucosa around the first and second premolars is visible.
- Hold the syringe caudad (towards the patients feet) and parallel to the premolars, with the needle’s bevel facing the mandible.
- At the buccal depression between the first and second premolars, advance the needle ~1cm.
- Aspirate to rule out intravascular placement.
- Administer 1-2mL of anesthetic.
Ear
Overview
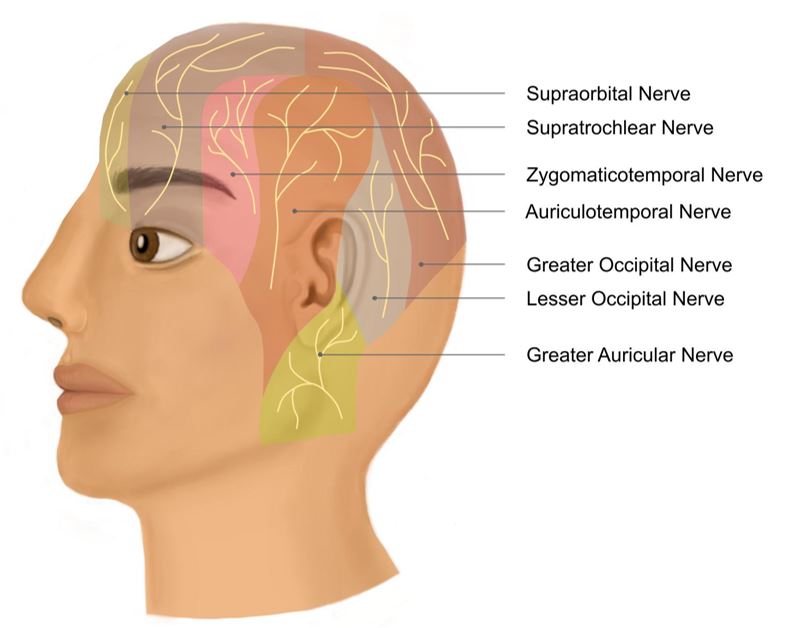
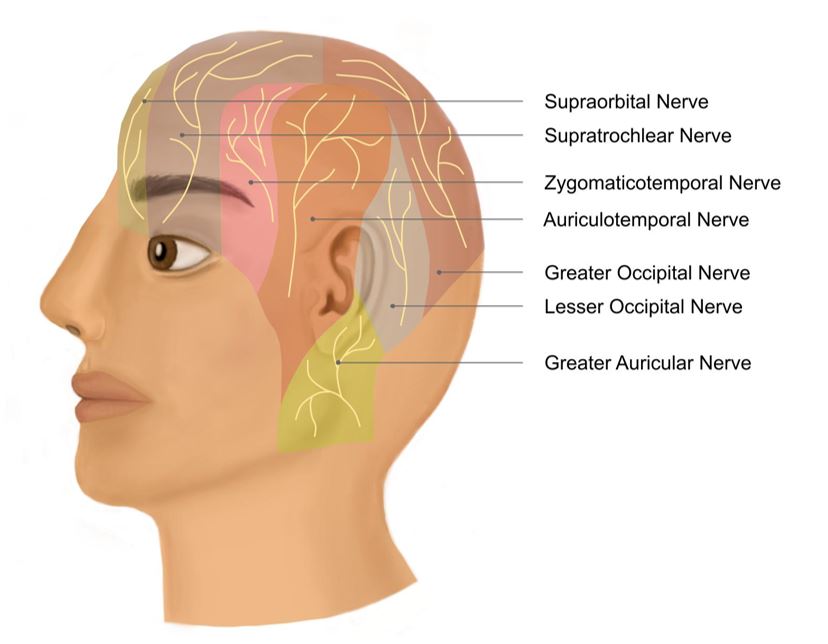
- Sensory innervation of the external ear is mediated by the greater auricular, lesser occipital, auriculotemporal and vagus (auricular branch) nerves.
- The distribution of sensory innervation from these nerves can vary substantially.
- Traditionally, the “ring block” technique has been employed to anesthetize each of the auriculotemporal, posterior auricular and greater auricular
- More recently, an ultrasound-guided greater auricular nerve block (UGANB) has been proposed for procedures involving the tail of the helix or lobule.
Greater Auricular
Injection Site | Slightly inferior and posterior to external auditory meatus (EAM)
Equipment | 10 ml syringe, 25 or 27 GA needle
Anesthetic | 5 ml, Lidocaine 2% w/ Epi or Bupivacaine 0.5%
Indications | Part of ring block
Contraindications | Inability to locate anatomical landmarks, pre-existing infection at site of injection, allergy to local anesthetic, lack of patient consent or cooperability
Considerations
- Usually performed in the ring block technique in conjunction with the lesser occipital and auriculotemporal nerve blocks.
Anatomy
- Greater auricular nerve penetrates the cervical fascia at the posterior border of the sternocleidomastoid muscle (SCM), approximately 6-7cm from the EAM.
- Nerve then travels anterosuperiorly towards the ear.
Technique
- Insert the needle 4-5cm away from and pointed towards the EAM.
- Advance the needle 3-4cm parallel to the skin.
- Aspirate and administer 1ml of anesthetic.
- Withdrawn the needle but stop short of fully removing it from the skin.
- Redirect the needle behind the ear, towards the mastoid process.
- Advance the needle 3-4cm parallel to the skin.
- Aspirate and administer 2ml of anesthetic as the needle is withdrawn, but again stop short of fully removing it from the skin.
- Redirect the needle towards the area anterior to the tragus.
- Advance the needle 3-4cm parallel to the skin.
- Aspirate and administer 2ml of anesthetic as the needle is fully withdrawn.
Lesser Occipital
Injection Site | Posterior to the insertion of SCM
Equipment | 3-10 ml syringe, 25 or 27 GA needle
Anesthetic | 2 ml, Lidocaine 2% w/ Epi or Bupivacaine 0.5%
Indications | Part of ring block
Contraindications | Inability to locate anatomical landmarks, pre-existing infection at site of injection, allergy to local anesthetic, lack of patient consent or cooperability
Considerations
- Usually performed in the ring block technique in conjunction with the greater auricular and auriculotemporal nerve blocks.
Anatomy
- Lesser occipital nerve penetrates the cervical fascia at the posterior border of the SCM, approximately 4-5cm from the EAM.
- Nerve then travels superiorly towards the ear.
Technique
- While pointed superiorly and slightly posteriorly, insert the needle posterior to the insertion point of the SCM.
- Aspirate and administer 2ml of anesthetic as the needle is withdrawn
Auriculotemporal
Injection Site | Anterior to tragus
Equipment | 3-10 ml syringe, 25 or 27 GA needle
Anesthetic | 2.5 ml, Lidocaine 2% w/ Epi or Bupivacaine 0.5%
Indications | Part of ring block
Contraindications | Inability to locate anatomical landmarks, pre-existing infection at site of injection, allergy to local anesthetic, lack of patient consent or cooperability
Considerations
- Usually performed in the ring block technique in conjunction with the greater auricular and auriculotemporal nerve blocks.
Anatomy
- Auriculotemporal nerve penetrates the cervical fascia slightly anterior to the tragus.
Technique
- Insert the needle slightly anterior to the tragus.
- Aspirate and administer 0.5ml of anesthetic.
- Withdrawn the needle but stop short of fully removing it from the skin.
- Redirect the needle superiorly and advance 3-4cm.
- Aspirate and administer 1ml of anesthetic.
Nose
Nasociliary
Injection Site | 1cm superior to medial canthus of eye
Equipment | 3-10 ml syringe, 25 or 27 GA needle (15-30mm)
Anesthetic | 2 ml, Lidocaine 2% w/o Epi or Bupivacaine 0.5%
Indications | Laceration repair of nasal skin
Contraindications | Inability to locate anatomical landmarks, pre-existing infection at site of injection, allergy to local anesthetic, lack of patient consent or cooperability
Considerations
- Usually performed in combination with infratrochlear nerve block.
Anatomy
- Nasociliary nerve originates from ciliary ganglion and quickly gives off its terminal branches, including anterior/posterior ethmoidal, long ciliary and infratrochlear
Technique
- Insert the needle ~1cm superior to the medial canthus, halfway between the eyebrow and posterior palpebral fold.
- Advance the needle ~1.5cm posteromedially.
- Aspirate and administer up to 2ml of anesthetic while slowly withdrawing the needle.
Mouth
Overview
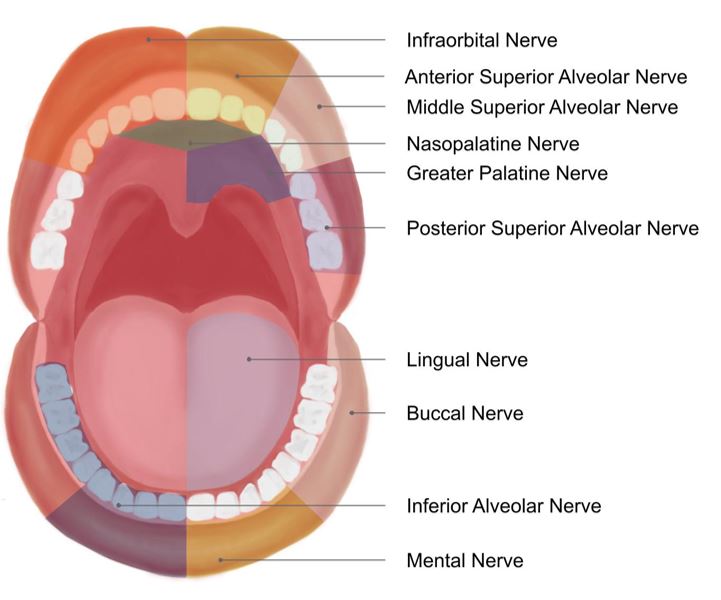
- Sensory innervation of the maxillary dentition is supplied by the anterior superior alveolar (ASA), middle superior alveolar (MSA) and posterior superior alveolar (PSA) nerves.
- The MSA may be present in only 30-72% of patients — in these cases, the ASA and PSA alone supply the sensory innervation.
- The ASA and MSA are branches of the infraorbital nerve — an RCT comparing combined nerve block of ASA/MSA to infraorbital nerve block demonstrated more successful anesthesia of incisors but less successful anesthesia of central incisors with the ASA/MSA block.
Anterior Superior Alveolar
Injection Site | Apex of canine
Equipment | 3-10 ml syringe, 25 or 27 GA needle (35 mm)
Anesthetic | 1-3 ml, Lidocaine 2% w/ Epi or Bupivacaine 0.5%
Indications | Anesthesia of maxillary central and lateral incisors (potentially premolars and mesiobuccal root of first molar in patients lacking MSA nerve)
Contraindications | Inability to locate anatomical landmarks, pre-existing infection at site of injection, allergy to local anesthetic, lack of patient consent or cooperability
Anatomy
- The ASA nerve branches off the infraorbital nerve proximal to the infraorbital foramen.
- The nerve then travels along the anterior wall of maxillary sinus to the anterior surface of maxilla before innervating central and lateral incisors.
Technique
- Retract the upper lip anteriorly and superiorly.
- Insert the needle at the mucosal reflection above the apex of the canine.
- Advance the needle superiorly and posteriorly at 45º.
- Aspirate and administer 2-3ml of anesthetic.
Middle Superior Alveolar
Injection Site | Mucosal fold between second premolar and first molar
Equipment | 3-10 ml syringe, 25 or 27 GA needle (35 mm)
Anesthetic | 1-3 ml, Lidocaine 2% w/ Epi or Bupivacaine 0.5%
Indications | Anesthesia of premolars and mesiobuccal root of first molar
Contraindications | Inability to locate anatomical landmarks, pre-existing infection at site of injection, allergy to local anesthetic, lack of patient consent or cooperability
Anatomy
- The MSA nerve branches off the infraorbital nerve proximal to the infraorbital foramen.
- The nerve then travels along the anterior wall of maxillary sinus to the anterior surface of maxilla before innervating premolars and mesiobuccal root of the first molar.
Technique
- Retract the upper lip anteriorly and superiorly.
- Insert the needle at the mucosal fold between the second premolar and first molar.
- Advance the needle superiorly and posteriorly at 45º.
- Aspirate and administer 2-3ml of anesthetic.
Posterior Superior Alveolar
Injection Site | Superior to root of second molar
Equipment | 3-10 ml syringe, 25 or 27 GA needle (35 mm)
Anesthetic | 1-3 ml, Lidocaine 2% w/ Epi or Bupivacaine 0.5%
Indications | Anesthesia of molars (potentially mesiobuccal root of first molar in patients lacking MSA nerve)
Contraindications | Inability to locate anatomical landmarks, pre-existing infection at site of injection, allergy to local anesthetic, lack of patient consent or cooperability
Anatomy
- The PSA nerve branches off the maxillary nerve proximal to the infraorbital foramen.
- The nerve then travels below the maxilla (not through the infraorbital foramen) to the lateral surface of the maxilla before innervating the molars (except for mesiobuccal root of first molar in patients with MSA nerve).
Technique
- Retract the upper lip anteriorly and superiorly.
- Insert the needle superior to the root of the second molar.
- Advance the needle superiorly and posteriorly at 45º, towards the maxillary tuberosity.
- When contact with bone is made, slightly retract the needle.
- Aspirate and administer 2-3ml of anesthetic.
Greater Palatine
Injection Site | Slightly anterior to greater palatine foramen
Equipment | 3-10 ml syringe, 25 or 27 GA needle (35mm)
Anesthetic | 1-3 ml, Lidocaine 2% w/ Epi or Bupivacaine 0.5%
Indications | Anesthesia of ipsilateral palatal tissues posterior to canine
Contraindications | Inability to locate anatomical landmarks, pre-existing infection at site of injection, allergy to local anesthetic, lack of patient consent or cooperability
Anatomy
- The greater palatine nerve branches off the maxillary nerve.
- The nerve passes through the greater palatine canal before exiting through the greater palatine foramen to innervate the ipsilateral palatal tissues posterior to the canine.
Technique
- Locate the greater palatine foramen, which lies medial to the area between the posterior half of the second molar to the anterior half of the third molar.
- With a cotton swab, apply pressure to greater palatine foramen until blanching occurs.
- Insert the needle 1-2mm anterior to the foramen.
- Slowly advance the needle while depositing small amounts of anesthetic.
- Once contact with bone is made, retract the needle slightly.
- Aspirate and administer 0.5ml of anesthetic over 30 seconds.
Nasopalatine
Injection Site | Slightly lateral to incisive papilla
Equipment | 3-10 ml syringe, 25 or 27 GA needle (short)
Anesthetic | 1-3 ml, Lidocaine 2% w/ Epi or Bupivacaine 0.5%
Indications | Anesthesia of bilateral palatal tissues anterior to canine
Contraindications | Inability to locate anatomical landmarks, pre-existing infection at site of injection, allergy to local anesthetic, lack of patient consent or cooperability
Anatomy
- The nasopalatine nerve is a branch of the maxillary nerve.
- The nerve travels through the pterygopalatine fossa and nasal cavity before exiting through the nasopalatine foramen to innervate the anterior palatal tissues.
Technique
- The right-handed practitioner stands on the patient’s right side and vice versa.
- With a cotton swab, apply pressure to incisive papilla until blanching occurs.
- While maintaining pressure, insert the needle just lateral to, and directed at, the incisive papilla. The bevel should point towards the tissue.
- Slowly advance the needle while depositing small amounts of anesthetic.
- Once contact with bone is made, retract the needle slightly.
- Aspirate and administer 0.5ml of anesthetic over 30 seconds.
Inferior Alveolar / Lingual
Injection Site | 3/4 of the distance between pterygomandibular raphe and coronoid notch, within the pterygomandibular depression
Equipment | 3-10 ml syringe, 25 or 27 GA needle
Anesthetic | 1-3 ml, Lidocaine 2% w/ Epi or Bupivacaine 0.5%
Indications | Laceration repair and excision of anterior tongue//lower lip, anterior buccal mucosa, mandibular/dental fracture, dental caries/abscess, dry socket
Contraindications | Inability to locate anatomical landmarks, pre-existing infection at site of injection, allergy to local anesthetic, lack of patient consent or cooperability
Considerations
- The inferior alveolar and lingual nerve blocks are often performed in the same injection.
- If exclusive lingual anesthesia is required, an isolated lingual nerve block provides better anesthesia vs combination with inferior alveolar nerve block according to a recent RCT.
- If anesthesia of the buccal mucosa adjacent to the molars and second premolar is required, the inferior alveolar nerve block will not be sufficient.
- Unlike other techniques such as the Gow-Gates, the inferior alveolar block is not a complete mandibular nerve block. Nonetheless, RCTs have demonstrated similar efficacy of both techniques in providing pulpal and gingival anesthesia.
Anatomy
- Inferior alveolar nerve enters the mandible via mandibular foramen, just posterior to the lingula.
- Inferior alveolar artery/vein travel alongside the nerve.
- Lingual nerve travels anterior to the inferior alveolar, along the anterior aspect of the mandibular ramus. Lingual nerve crosses into the floor of the mouth at the approximate level of the molars.
- Needle insertion is directed towards the lingula. The needle should pass posteromedially to the lingual nerve and just anterior to the inferior alveolar nerve.
Technique
- Ask the patient to open their mouth wide.
- Use the index finger to palpate the posterior border of the mandible.
- Use the thumb to palpate the coronoid notch intraorally.
- Direct the needle to a position 3/4 of the way from the coronoid notch to the pterygomandibular raphe.
- Rest the body of the syringe on the patient’s first premolar.
- The needle should lie parallel to and ~1cm above the occlusal plane of the molars.
- Advance the needle until contact with the mandibular ramus.
- Note: Paresthesia indicates contact with the inferior alveolar nerve and correct trajectory. Slightly withdraw the needle and redirect while maintaining trajectory towards the mandibular ramus.
- Withdraw 1mm and aspirate to rule out intravascular placement.
- Note: If intravascular placement is revealed, withdraw 2-3mm and re-aspirate before administering anesthetic.
- Administer 1-3mL of anesthetic. Withdraw the needle halfway and administer another 1mL of anesthetic to block the lingual nerve.
Scalp
Overview
- The complete scalp block consists of six separate nerve blocks: supraorbital, supratrochlear, auriculotemporal, zygomaticotemporal, greater auricular and lesser and greater occipital.
- Zygomaticotemporal and greater occipital nerve blocks are described below — all others are described in the sections above.
- Consider using a subset of these nerve blocks depending on the area requiring anesthesia.
Zygomaticotemporal
Injection Site | Posterior to lateral orbital rim at level of lateral canthus
Equipment | 3-10 ml syringe, 25 or 27 GA needle
Anesthetic | 1-2 ml, Lidocaine 2% w/ Epi or Bupivacaine 0.5%
Indications | Persistent headaches, anesthesia of anterior temporal region or as part of scalp block
Contraindications | Inability to locate anatomical landmarks, pre-existing infection at site of injection, allergy to local anesthetic, lack of patient consent or cooperability
Anatomy
- The zygomaticotemporal nerve is a branch of the zygomatic nerve, which itself originates from the maxillary nerve.
- The zygomaticotemporal nerve courses through the temporal fossa before penetrating the temporal fascia 2cm superior to the zygomatic arch and innervating the anterior component of the temporal region.
Technique
- With the patient supine, palpate the posterolateral aspect of the lateral orbital rim.
- Insert the needle slightly posterior to the lateral orbital rim at the level of the lateral canthus.
- Advance the needle towards the lateral orbital rim until contact with bone is made.
- Aspirate and administer 1-2ml of anesthetic
Greater Occipital
Injection Site | ~2cm lateral and inferior to occipital protuberance
Equipment | 3-10 ml syringe, 25 or 27 GA needle (35mm)
Anesthetic | 2 ml, Lidocaine 2% w/ Epi or Bupivacaine 0.5%
Indications | Occipital neuralgia, anesthesia of posterior scalp
Contraindications | Inability to locate anatomical landmarks, pre-existing infection at site of injection, allergy to local anesthetic, lack of patient consent or cooperability
Anatomy
- The greater occipital nerve is a branch of the dorsal ramus of C2, originating between the C1 and C2 vertebrae.
- The nerve ascends along the occiput to supply the posterior scalp.
Technique
- With the patient seated and their neck slightly flexed, palpate for the occipital protuberance and mastoid process.
- If occipital neuralgia is suspected, the greater occipital nerve may be localized using Tinel’s test.
- Verify the location of the occipital artery, which should be readily palpable lateral to the occipital protuberance.
- Insert the needle ~2cm lateral and inferior to the occipital protuberance, avoiding the occipital artery (the nerve and injection site should be medial to the artery).
- If contact with the skull is made, slightly withdraw the needle.
- Administer 2ml of anesthetic
Related Information
Reference List
Malik A, Thom S, Haber B, Sarani N, Ottenhoff J, Jackson B et al. Regional Anesthesia in the Emergency Department: an Overview of Common Nerve Block Techniques and Recent Literature. Curr Emerg Hosp Med Rep. 2022;10:54-66. Available from: https://sjrhem.ca/wp-content/uploads/2023/10/s40138-022-00249-w.pdf
Sola C, Dadure C, Choquet O, Capdevila X. Nerve Blocks of the Face [Internet]. NYSORA [cited 2024 May 03]. Available from: https://www.nysora.com/techniques/head-and-neck-blocks/nerve-blocks-face/
Gleeson AP & Gray AJ. Management of retained ear-rings using an ear block. J Accid Emerg Med. 1995;12:199-201. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1342480/pdf/jaccidem00008-0039.pdf
Valesco I & Soto R. Anterior and middle superior alveolar nerve block for anesthesia of maxillary teeth using conventional syringe. Dent Res J (Isfahan). 2012;9(5):535-540. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3612188/
Umamaheswara Rao GS. Precise scalp block – have another look at scalp innervation. J Neurosci Rural Pract. 2023;14(1):1-2. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9944308/
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jun 13, 2025
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.