Diagnosis of STEMI Equivalents
Cardiovascular
Overview
- De Winter’s T waves
- Anterior STEMI equivalent.
- Indicative of early or evolving proximal left anterior descending (LAD) occlusion.
- ECG: Upsloping ST-segment depression (STD) in V1-V6 with prominent and symmetrical T-wave.
- Wellens’ syndrome
- Anterior STEMI equivalent.
- Indicative of critical stenosis of the proximal LAD and imminent anterior infarct.
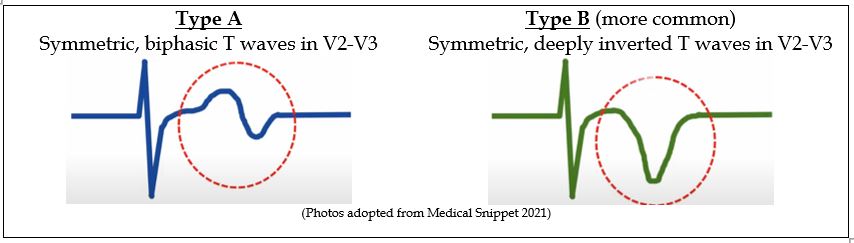
- ECG: Symmetrical T waves with deep inversion or biphasicity in V2-V3.
- ST-elevation in lead aVR
- Anterior STEMI equivalent.
- Indicative of proximal left main (LM) or left anterior descending coronary artery occlusion; or subendocardial ischemia due to subtotal occlusion or triple vessel disease; or a repolarization abnormality.
- ECG: ST-elevation >1mm in aVR with reciprocal anterolateral STD suggests LM or LAD occlusion, whereas without reciprocal STD is more suggestive of subtotal. occlusion (ie: demand etiology or triple vessel disease).
- Acute MI in the presence of Left Bundle Branch Block (LBBB)
- New LBBB is no longer considered a STEMI equivalent.
- Several tools have been developed to help identify ischemia and diagnose STEMI in patients with LBBB or ventricular paced rhythms.
- Sgarbossa Criteria (1996) – A highly specific, but insensitive point scoring system with 3 criteria (concordant STE, concordant STD, and excessive discordance).
- Smith-Modified Sgarbossa Criteria (2012) – Improved the sensitivity and diagnostic accuracy by changing the 3rd criteria to a ratio rather than a measurement and eliminating the point scoring.
- BARCELONA Criteria (2020) – Further improved the sensitivity and diagnostic accuracy with changes to both the 2nd and 3rd.
Management
De Winter’s T waves
- Background:
- Anterior STEMI equivalent indicative of an early or evolving proximal LAD occlusion.
- History and Physical:
- Findings suggestive of acute coronary syndrome (ACS).
- ECG findings:
- Concave upsloping STD (>1mm) in V1to V6 with prominent symmetrical T waves.
- Reciprocal 1-2mm STE in aVR is common.
- QRS complexes are usually normal or slightly wide.
- Loss of R-wave progression can occur.
The following table compares De Winter’s T-waves to non-ischemic STE and STEMI:
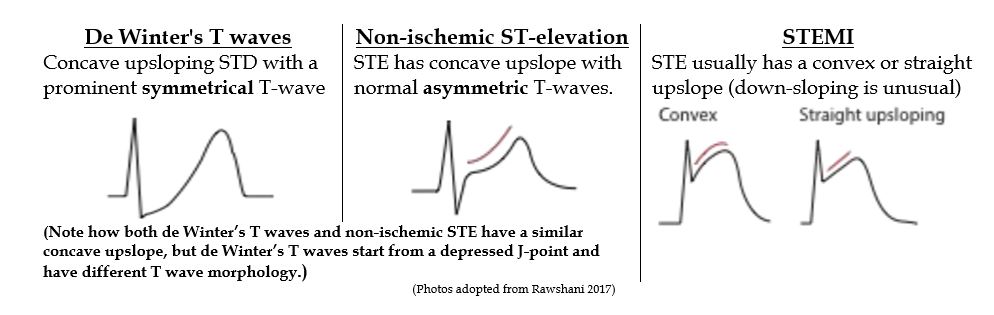
(Photos adopted from Rawshani 2017)
- Recommended Treatment:
- Treat as ACS; these lesions result in extensive anterior infarction and patients require urgent cardiology consultation and revascularization intervention.
Wellens’ syndrome (aka “The Widow Maker”)
- Background:
- Anterior STEMI equivalent with high specificity for critical stenosis of the proximal LAD.
- History and Physical:
- Patients are typically pain-free at the time of ECG and will have normal or mildly elevated biomarkers.
- ECG findings:
- Symmetrical deeply inverted (Type A) or Biphasic (Type B) T-waves in V2 & V3,
- No STE (<1 mm when measured at the J-point),
- No precordial Q waves, and
- Normal R wave progression (R amplitude in V3 >3mm).
- Recommended Treatment:
- Treat as ACS and patients require admission, urgent Cardiology consultation, and revascularization as they are at extreme risk (~75% in <2weeks) of developing massive anterior infarction.
ST-elevation in lead aVR
- Background:
- aVR was designed to evaluate the right upper heart (RV outflow tract & basal interventricular septum).
- STE >1mm in aVR may represent:
- a STEMI equivalent indicating occlusion of the left main (LM) or proximal LAD arteries; or
- widespread subendocardial ischemia due to near-total LM occlusion, triple vessel disease, or demand etiology; or
- a repolarization abnormality due to LVH or electrolyte imbalances.
- History and Physical:
- Findings suggestive of ACS.
- ECG findings:
- STE in aVR >1mm with diffuse reciprocal STD indicates acute LM or proximal LAD occlusion. The following ECG depicts an acute LM occlusion with STE in aVR (blue arrow) and concomitant diffuse reciprocal ST-depressions:
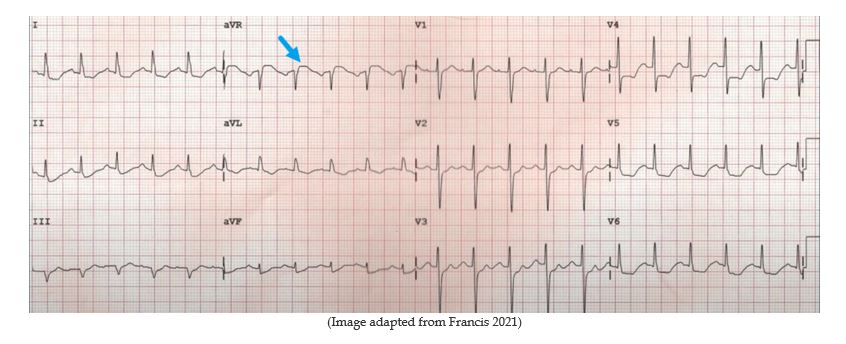
-
- STE in aVR >1mm without diffuse STD can also indicate proximal occlusion, but is more likely secondary to widespread subendocardial ischemia due to severe nonocclusive LM disease, triple vessel disease, or demand etiology (i.e., tachycardia, hypo-or hypertension, aortic stenosis, etc.)
- STE in aVR >1mm in the presence of tachycardia is almost always due to a supply-demand mismatch and not suggestive of LM occlusion.
- STE in aVR > V1 usually differentiates LM from proximal LAD occlusion.
- Recommended Treatment:
- Recognizing this finding is critical because the LM supplies ~75% of the LV myocardium and its occlusion would result in significant mortality.
- LM occlusions are heterogeneric and may also present with concomittent anterolateral ST elevation or ischemia-induced conduction disturbances.
Acute MI in the presence of LBBB:
- Background:
- A new LBBB is no longer recognized as STEMI equivalent or indication for revascularization, but guidelines still suggest they be carefully considered and interpreted in clinical context.
- Several clinical decision tools have been developed to help identify ischemia and diagnose acute MI in patients with abnormal repolarization due to LBBB or ventricular pacing.
- The Original Sgarbossa Criteria (1996)
- ≥ 3 points are required to diagnose acute myocardial infarction (Sn 36%; Sp 96%):
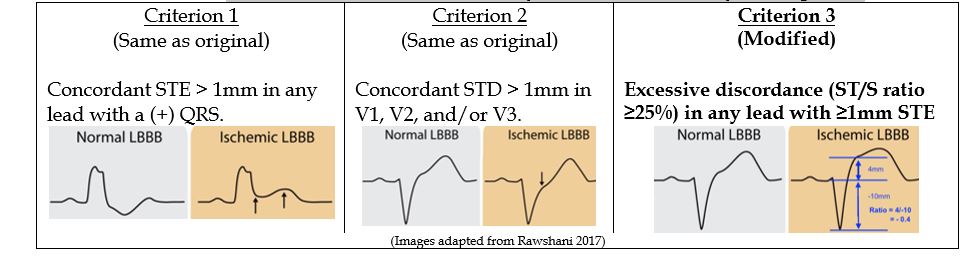
- Criterion 1: Concordant STE ≥ 1mm in any lead with a (+) QRS (5 points).
- Criterion 2: Concordant STD >1mm in V1-V3 (3 points).
- Criterion 3: Excessive discordance (≥ 5 mm) in any lead with STE (2 points).
- Overall use was limited by poor sensitivity and inability to rule out ischemia.
- ≥ 3 points are required to diagnose acute myocardial infarction (Sn 36%; Sp 96%):
- The Smith-Modified Sgarbossa Criteria (2012)
- Made two major changes to improve sensitivity and offer better diagnostic accuracy (Sn 90%; Sp 90%):
- Point scoring was eliminated which allowed for the diagnosis of MI to be made if any of the criterion were met.
- The 3rd criterion measuring excessive ST discordance would use an ST/S ratio >25% rather than the arbitrary >5mm cut-off used by the original.
- Made two major changes to improve sensitivity and offer better diagnostic accuracy (Sn 90%; Sp 90%):
- The BARCELONA Criteria (2020)
- Further improved sensitivity and diagnostic accuracy (Sn 93%; Sp 94%) by changing both the 2nd and 3rd.
- Criterion 1: (unchanged) Concordant STE > 1mm in any lead with a (+) QRS.
- Criterion 2: Concordant STD >1mm in any lead (instead of relying on just V1-V3 per the Smith-modified Criteria).
- Criterion 3: Excessive discordance was changed to use ST deviation ≥ 1mm in any lead where the dominant R or S is ≤ 6mm (instead of using the ST/S ratio >25% per the Smith-modified Criteria). This change now allowed for assessment of leads when they are low voltage.
- The BARCELONA criteria have not yet been externally validated.
- Further improved sensitivity and diagnostic accuracy (Sn 93%; Sp 94%) by changing both the 2nd and 3rd.
Related Information
Reference List
Rawshani, A. Clinical ECG Interpretation: T-waves in ischemia: hyperacute, inverted (negative), Wellens’ sign & de Winter’s sign. (Section 3, Chapter 13). 2017. Accessed Dec 1, 2023. https://ecgwaves.com/topic/t-wave-negative-inversions-hyperacute-wellens-sign-de-winters/. Accessed Dec 1, 2023.
McLaren J. ECG Cases 21: Hyperacute T-waves and Occlusion MI. Emergency Medicine Cases. 2021. Accessed Dec 1, 2023. https://emergencymedicinecases.com/hyperacute-t-waves-occlusion-mi/
Somers MP, Brady WJ, Perron AD, Mattu A. The prominent T wave: electrocardiographic differential diagnosis. Am J Emerg Med. 2002;20(3):243-251. doi:10.1053/ajem.2002.32630
O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. JACC January 29, 2013;61(4):378-140
Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines [published correction appears in Circulation. 2021 Nov 30;144(22):e455]. Circulation. 2021;144(22):e368-e454. doi:10.1161/CIR.0000000000001029
Gregory D, Wexler B, Becker B. De Winter T-wave Pattern in Proximal Left Anterior Descending Artery Occlusion. Clin Pract Cases Emerg Med. 2020;4(3):476-477. doi:10.5811/cpcem.2020.5.47322
R.J. De Winter, N.J.W. Verouden, H.J.J. Wellens, A.A.M. Wilde. A new ECG sign of proximal LAD occlusion. N Engl J Med, 359 (19) (2008), pp. 2071-2073, 10.1056/NEJMc0804737
Littmann L. The Dressler – de Winter sign of acute proximal LAD occlusion. J Electrocardiol. 2018;51(1):138-139. doi:10.1016/j.jelectrocard.2017.08.024
Pendell Meyers H, Bracey A, Lee D, et al. Accuracy of OMI ECG findings versus STEMI criteria for diagnosis of acute coronary occlusion myocardial infarction. Int J Cardiol Heart Vasc. 2021;33:100767. Published 2021 Apr 12. doi:10.1016/j.ijcha.2021.100767
Miranda DF, Lobo AS, Walsh B, Sandoval Y, Smith SW. New Insights Into the Use of the 12-Lead Electrocardiogram for Diagnosing Acute Myocardial Infarction in the Emergency Department. Can J Cardiol. 2018;34(2):132-145. doi:10.1016/j.cjca.2017.11.011
Al-Assaf O, Abdulghani M, Musa A, AlJallaf M. Wellen’s Syndrome: The Life-Threatening Diagnosis. Circulation. 2019;140(22):1851-1852. doi:10.1161/CIRCULATIONAHA.119.043780
Rhinehardt J, Brady WJ, Perron AD, Mattu A. Electrocardiographic manifestations of Wellens’ syndrome.Am J Emerg Med. 2002; 20:638–643. doi: 10.1053/ajem.2002.34800
de Zwaan C, Bär FW, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction.Am Heart J. 1982; 103:730–736. doi: 10.1016/0002-8703(82)90480-x
de Zwaan C, Bär FW, Janssen JH, Cheriex EC, Dassen WR, Brugada P, Penn OC, Wellens HJ. Angiographic and clinical characteristics of patients with unstable angina showing an ECG pattern indicating critical narrowing of the proximal LAD coronary artery. Am Heart J. 1989; 117:657–665. doi: 10.1016/0002-8703(89)90742-4
Medical Snippet. Wellens Syndrome with ECG and Angiography example [Video]. Youtube. https://www.youtube.com/watch?app=desktop&v=csL3xCRU6bU. Pub May 17, 2020. Accessed Dec 1, 2023.
Francis J. Importance of Lead aVR [Video]. Youtube. https://www.youtube.com/watch?v=btTHkjF3oFA&t=287s. Pub Apr 5, 2021. Accessed Dec 1, 2023.
Tamura A. Significance of lead aVR in acute coronary syndrome. World J Cardiol. 2014;6(7):630-637. doi:10.4330/wjc.v6.i7.630
Brouner M, Hammock J, Doppalapudi H. Does ST Elevation in Lead aVR Require an Emergent Trip to the Catheterization Laboratory? JAMA Intern Med. 2023;183(3):261–262. doi:10.1001/jamainternmed.2022.5901
Rawshani, A. Clinical ECG Interpretation: T-waves in ischemia: hyperacute, inverted (negative), Wellens’ sign & de Winter’s sign. (Section 3, Chapter 13). 2017. Accessed Dec 1, 2023. https://ecgwaves.com/topic/t-wave-negative-inversions-hyperacute-wellens-sign-de-winters/. Accessed Dec 1, 2023.
Smith SW, Dodd KW, Henry TD, Dvorak DM, Pearce LA. Diagnosis of ST-elevation myocardial infarction in the presence of left bundle branch block with the ST-elevation to S-wave ratio in a modified Sgarbossa rule [published correction appears in Ann Emerg Med. 2013 Oct;62(4):302]. Ann Emerg Med. 2012;60(6):766-776. doi:10.1016/j.annemergmed.2012.07.119
Meyers HP, Limkakeng AT Jr, Jaffa EJ, et al. Validation of the modified Sgarbossa criteria for acute coronary occlusion in the setting of left bundle branch block: A retrospective case-control study. Am Heart J. 2015;170(6):1255-1264. doi:10.1016/j.ahj.2015.09.005
Di Marco A, Rodriguez M, Cinca J, et al. New Electrocardiographic Algorithm for the Diagnosis of Acute Myocardial Infarction in Patients With Left Bundle Branch Block [published correction appears in J Am Heart Assoc. 2020 Nov 17;9(22):e014618]. J Am Heart Assoc. 2020;9(14):e015573. doi:10.1161/JAHA.119.015573
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Feb 03, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.