Disseminated Intravascular Coagulopathy (adults)
Cardiovascular, Critical Care / Resuscitation, Hematological / Oncological, Infections, Inflammatory, Pregnancy, Trauma
First 5 Minutes
Initial assessment (1-4)
- Is the patient stable or unstable?
- Perform ABCDE assessment.
- If unstable, start a “MOVIE” (monitors, oxygen, vitals, large bore IV access/investigations, ECG).
- What is the underlying cause?
- Start treating it.
- Collect blood to monitor coagulation factors.
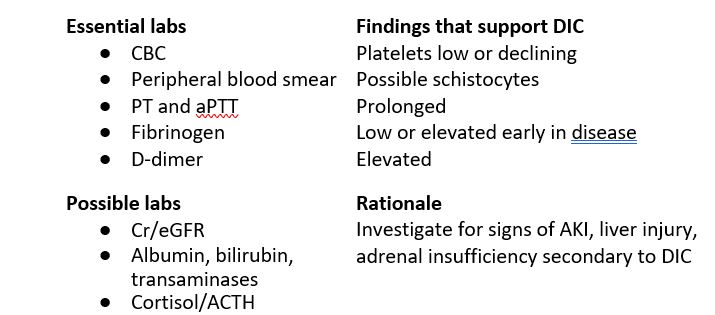
| Essential labs
CBC Peripheral blood smear PT and aPTT Fibrinogen D-dimers |
→ Findings in DIC
→ Platelets low or declining → Possible schistocytes → Prolonged → Low or elevated early in disease → Elevated |
- Supportive care and prepare for patient deterioration.
- Keep patient warm (give blankets, warm room, warm any IV fluids).
- Prepare for red cell, platelet, FFP transfusions.
- Measure blood losses.
For pregnant patients, notify obstetrics team early on. Delivery may be component of management.
Context
Background (1,2,5-8)
- Definition
- Acquired coagulation disorder leading to widespread bleeding and clotting.
- Infectious and non-infectious causes.
- Strong mortality predictor.
- Prevention is essential.
- Suspect DIC in patients with known DIC-causing disease processes.
- Causes
- Infection ± sepsis (50% of DIC cases).
- Head trauma (45% of patients with head injury, burns can develop DIC).
- Giant hemangiomas.
- Cancers (solid and leukemias).
- Major surgery.
- Obstetrical causes (especially placental abruption, pre-eclampsia).
- MAHAs (TTP, HUS, chemotherapy-induced, malignant HTN, HELLP syndrome).
- Severe immune or toxic reactions.
- Snake bite.
- Pathophysiology
- Trigger (infection, immune, trauma, etc.)→ Pro-inflammatory state (IL-6, TNF-a)→ Widespread platelet activation
→ Disproportionate platelet/coagulation factor consumption
→ Endothelial dysfunction
→ Vascular leakage, edema
- Small vessel ischemia-reperfusion injury → can lead to multi-organ failure
- Endothelial dysfunction + anticoag issues → thrombin activation (fibrin activation)
- Trigger (infection, immune, trauma, etc.)→ Pro-inflammatory state (IL-6, TNF-a)→ Widespread platelet activation
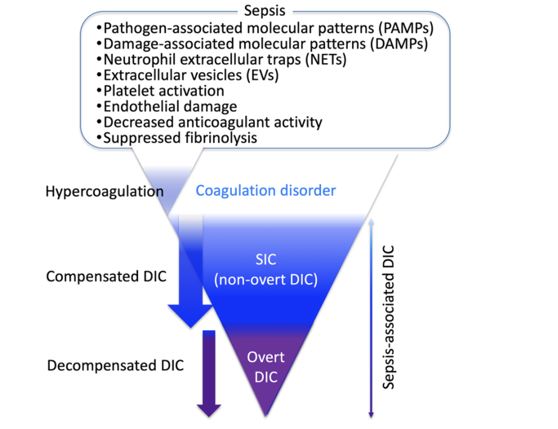
Image source: The pathophysiology, diagnosis, and management of sepsis-associated disseminated intravascular coagulation.
Diagnostic Process
Diagnosis (1-5)
Clinical and lab-based diagnosis
- DDx
- Liver disease – looks same in labs, so rule out with clinical exam, Hx.
- Heparin-induced thrombocytopenia (HIT) – recent heparin administration.
- Thrombotic microangiopathy (TMA) – usually normal coagulation markers, platelets.
- Hemophagocytic lymphohistiocytosis (HLH) – results from uncontrolled immune activation, treatment targets.
- History
- Presence of known DIC-related disease process?
- Bleeding and clotting history.
- Urination history (kidney injury)?
- Dyspnea or hemoptysis (lung injury)?
- Neurological ROS.
Physical Exam
- Bleeding signs
- Petechiae, ecchymoses.
- Mucosal bleeding.
- Bleeding at sites of line or device insertions.
- Post-op bleeding.
- Thrombotic signs
- VTE.
- Reduced organ or limb perfusion secondary to thrombosis.
- Signs of endocarditis.
- Organ dysfunction signs
- Jaundice (liver injury)?
- Neurological screen.
- Purpura fulminans (cutaneous necrosis, widespread tissue thrombosis).

Purpura fulminans in septic shock patient. Source: https://emcrit.org/ibcc/pf/
- Labs
- Perform serial labs to track degree of coagulation, fibrinolysis.
-
- Calculator: Consider using DIC Score calculator to assess likelihood of DIC (based on platelet count, fibrin markers, PT time, fibrinogen).
Recommended Treatment
Management (1-4)
- Continue initial stabilization measures.
- Treat underlying condition
- Sepsis → 2 sets blood cultures draw, then broad spectrum Abx; consider anticoagulation (thrombomodulin or antithrombin).
- Trauma → stabilize other injuries. Consider TXA.
- Pregnancy → Consult OB/GYN. Give tranexamic acid early (1 g over 10 min IV, repeat if bleeding still at 30 min).
- Consult specialists as needed.
- Tailor DIC treatment according to presentation.
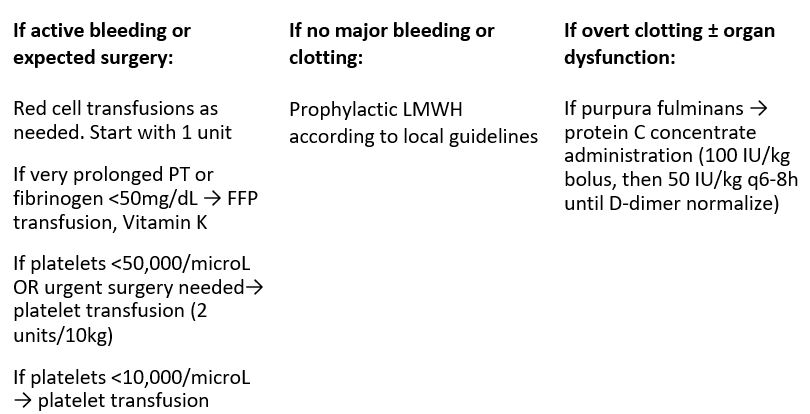
- Provide supportive measures for everyone
- Volume resuscitation where needed.
- Ventilatory support where needed.
- LMWH for DVT prophylaxis according to local guidelines.
Additional considerations for pregnant patients.
Unstable patient
- Call for help – notify obstetrics, anesthesia, neonatology, transfusion medicine.
- Oxygen – Maintain SpO2 ≥95%.
- Transfusions – group/screen/cross-match blood. 1:1:1 of red cells to plasma to platelets (O- blood at first, switch to cross-matched blood next).
- Fluids – Crystalloid and/or blood products to maintain MAP ≤65 mmHg, urine output ≥0.5ml/kg/h (blood ideal but lactated ringers can be used first if no blood available).
- Maintain warmth – give blankets, warm any IV fluids.
- Drugs – give TXA early (1 g over 10 min IV, repeat if bleeding still at 30 min).
- Coagulation monitoring (CBC, PT/aPTT, fibrinogens, FDPs).
- Hb ≥7 g/dL
- Fibrinogen ≥200 mg/dL
- Platelets ≥50,000/microL
- PT, aPTT <1.5x control
- Monitor fetus
Stable patient
- Monitor coagulation panel
- If fibrinogen <200 mg/dL AND active or expected bleeding, then give fibrinogen concentrate to get level >300 mg/dL.
- Expect uterine bleeding and manage it. Group/screen/cross-match blood. Consult obstetrics to make delivery decisions.
- Monitor fetus
Criteria For Hospital Admission
- Patient is unstable.
- Patient presented with overt DIC and coagulation profile hasn’t resolved (can take days).
- Requires continued interventions or frequent monitoring (e.g., IV medications or supportive care, non-improving DIC lab markers, transfusions indicated).
- Risk factors for poor prognosis: older age, severe organ injury, persistent hematological disturbances.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Moderate quality evidence due to variable causes and management approaches of DIC.
Related Information
OTHER RELEVANT INFORMATION
DIC Score – Assess likelihood of disseminated intravascular coagulation (DIC) (from International Society of Thrombosis and Hemostasis consensus guidelines.
Sepsis-Induced Coagulopathy (SIC) Score
Bloody Easy Coagulation Handbook – Transfusion Ontario
Reference List
Wang H. Disseminated intravascular coagulation – Symptoms, diagnosis and treatment. BMJ Best Practice US [Internet]. Kaye A, Toh CH, editors. BMJ Best Practice. 2021 [cited 2024 Apr 16]. Available from: https://bestpractice.bmj.com/topics/en-gb/184?q=Disseminated%20intravascular%20coagulation&c=recentlyviewed
Tintinalli JE, O. John Ma, Yealy D, Meckler GD, J. Stephan Stapczynski, Cline DM, et al. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 9th edition. McGraw Hill Professional; 2019.
Belfort M. UpToDate [Internet]. Lockwood C, Hepner D, Leung L, Uhl L, Barss V, editors. www.uptodate.com. 2024 [cited 2024 May 2]. Available from: https://www.uptodate.com/contents/disseminated-intravascular-coagulation-dic-during-pregnancy-clinical-findings-etiology-and-diagnosis?topicRef=1306&source=see_link
Belfort M. UpToDate [Internet]. Lockwood C, Hepner D, Leung L, Uhl L, Barss V, editors. www.uptodate.com. 2024 [cited 2024 May 2]. Available from: https://www.uptodate.com/contents/disseminated-intravascular-coagulation-dic-during-pregnancy-management-and-prognosis?search=dic%20pregnancy&source=search_result&selectedTitle=1%7E150&usage_type=default&display_rank=1#topicContent
Iba T, Helms J, Connors JM, Levy JH. The pathophysiology, diagnosis, and management of sepsis-associated disseminated intravascular coagulation. Journal of Intensive Care. 2023 May 23;11(1):24.
Levi M, de Jonge E, van der Poll T, ten Cate H. Disseminated intravascular coagulation. Thrombosis and haemostasis. 1999;82(08):695-705.
Disseminated intravascular coagulation. Nature Reviews Disease Primers. 2016 Jun 2;2(1).
Leung L. Evaluation and management of disseminated intravascular coagulation (DIC) in adults [Internet]. Mannucci P, Tirnauer J, editors. UptoDate; 2023 [cited 2024 Apr 16]. Available from: https://www.uptodate.com/contents/evaluation-and-management-of-disseminated-intravascular-coagulation-dic-in-adults?search=Disseminated%20intravascular%20coagulation%3A%20an%20update%20on%20pathogenesis%20and%20diagnosis.&source=search_result&selectedTitle=1%7E150&usage_type=default&display_rank=1#references
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated May 03, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.