Epistaxis – Diagnosis
Cardinal Presentations / Presenting Problems, Ears, Eyes, Nose, and Throat, Hematological / Oncological
Context
- 6% of adults require treatment for a nosebleed in their lifetime.
- Bimodal age distribution: 2-10 years and 50-80 years.
- 85% of the time the cause is unclear:
- Regional factors:
- Trauma (finger, FB, NG tube insertion).
- Nasal dryness and irritation (cold air, supplemental O2, rhinitis).
- Topical nasal medications (corticosteroids and antihistamines).
- Drugs (inhalants, cocaine).
- Nasopharyngeal neoplasm.
- Systemic risk factors and/or exacerbators:
- Coagulopathies (acquired or inherited).
- Anticoagulants and antiplatelets.
- Alcohol use disorder.
- Vascular abnormalities (i.e. hereditary hemorrhagic telangiectasia).
- Hypertension (uncertain association, may prolong bleeding).
- Congestive heart failure.
- Regional factors:
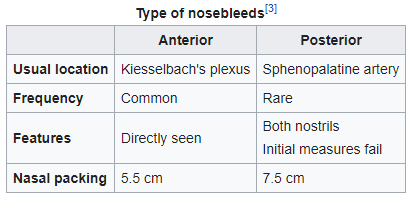
- Source of bleeding:
- Approach focuses on:
- Severity of bleeding:
- Hemodynamic stability.
- Initial hemostasis.
- Identifying the source of bleeding.
- Consider red flag diagnoses:
- Anticoagulated patient with supratherapeutic INR.
- Nasopharyngeal neoplasm.
- Posterior bleed secondary to carotid artery aneurysm.
- Severity of bleeding:
Diagnostic Process
- Assess airway compromise and hemodynamic stability
- Secure airway,
- IV fluid resuscitation,
- emergency ENT consult if needed
- History (2):
- Laterality and severity of bleeding
- Recurrent epistaxis
- Contributing factors and triggers (see above)
- Visualize the source of bleeding
Pretreatment
- Topical anesthetic and vasoconstrictor (5)
- Apply with cotton balls or with rolled cotton pledgets.
- Several options:
- Lidocaine (2 or 4%) with oxymetazoline spray (6)
- LET solution (lidocaine 4%, epinephrine 0.1%, and tetracaine 0.4%)
- 4% cocaine hydrochloride (both anesthetic and vasoconstrictive) (3)
- Apply pressure to attempt initial tamponade
- Patient may apply pressure for 10-15 minutes OR
If bleeding stops, observe for 30 mins – 1 hour with ambulation, and discharge home with instructions (see PECS – Epistaxis management).
If bleeding does not resolve:
- Optimize exposure (1) :
- Headlight, nasal speculum
- Clear the nose with blowing and/or suctioning
- Patient in “sniff” position
- Inspect:
- Kiesselbach’s plexus (anterior epistaxis)
- If no source of bleeding visualized:
- Either posterior epistaxis or resolving anterior epistaxis
- Proceed to treatment (see PECS – Epistaxis management)
- Investigations
Labs usually not required unless (3,7):
- CBC for heavy, recurrent bleeding, or suspected thrombocytopenia
- INR, PTT
- taking Warfarin
- taking DOAC and moderate to severe bleeding secondary to uncontrolled posterior epistaxis (8,9)
- known hepatic or renal dysfunction
- Creatinine, if DOAC (renally cleared) and significant bleeding (9)
- ECG, group and screen, crossmatch if blood loss significant (8).
- Clinical pitfalls
- Not investigating recurrent unilateral epistaxis for nasopharyngeal neoplasm
- CT and/or endoscopy (2)
- Higher risk if Chinese or South Asian decent
- Not involving ENT early for severe, refractory hemorrhage.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Established approach to common emergency department presentation.
Additional Resources
Useful links:
- BC Emergency Physician’s Network, PECS – Epistaxis Treatment in Adults
- ACEP now – Treatment of epistaxis
- ACEP – Approach flow chart (“Dundee” protocol)
- UptoDate – Management and treatment of epistaxis.
- Life In The Fast Lane: Epistaxis
- Epistaxis management in the Emergency Department (ALiEM)
Patient resources:
Related Information
Reference List
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Aug 04, 2020
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…





POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.