Hand & Finger Dislocation
Orthopedic, Trauma
First 5 minutes
- Initial management: [1] [2]
- Clean and cover open wounds.
- Remove constrictions (i.e., jewelry, watch, gloves, etc.) and assess neurovascular status. and compartment pressure (compartment syndrome).
- Pain management following neurological assessment (digital nerve or metacarpal block).
- Acute Carpal Tunnel Syndrome in the context of trauma is a surgical emergency [3] [4]
- Constant and severe pain and dysesthesias in median nerve distribution.
- Progressive rapid onset course over hours.
Context
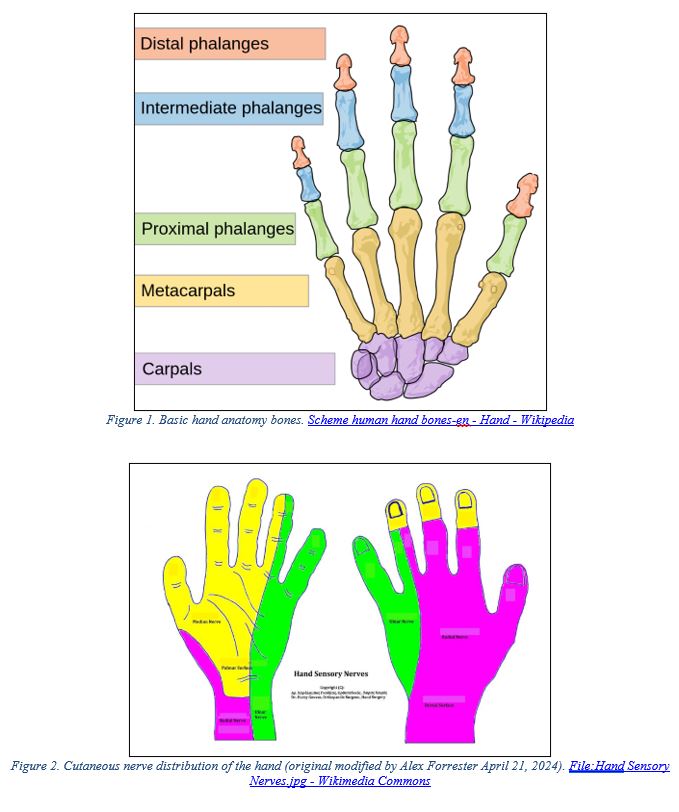
Understanding hand anatomy is important for recognizing and diagnosing hand and finger dislocations.
- Finger Dislocations (phalanges): [5]
- Three joints involved are metacarpophalangeal joint (MCP), proximal interphalangeal joint and distal interphalangeal joint (DIP).
- Dislocations may be in the dorsal, volar, or lateral planes.
- MCL dislocations typically result from hyperextension or high energy axial load.
- PIP dislocations are most common due to sports related injuries “coach’s finger.”
- DIP dislocations typically associated with fractures and skin injuries.
- Finger arteries and nerves run along volar aspect of finger.
- Hand Dislocations (metacarpal): [6] [7]
- Carpometacarpal (CMC) dislocations are rare, < 1% of all hand injuries.
- 4th and 5th metacarpal most often involved.
- Often associated with high impact collision or punching.
- Likely require surgical treatment with Kirschner wires (K-wires) for fixation or open reduction.
Diagnostic Process
- History: [3] [5]
- Mechanism of Injury (MOI)
- Handedness
- Previous Finger / Wrist Injuries
- Occupation / Hobbies / Sports
- Hand Exam: [3] [5] [8] [9]
- Visual inspection for open wounds, deformity, discoloration, swelling and atrophy.
- Use tourniquet or anesthetic with epinephrine to ensure a bloodless field for exam.
- Move fingers / wrist through complete range of motion (ROM).
- Palpate to determine location of maximal tenderness.
- For fingers, test hyperextension (volar plate integrity), lateral stresses (collateral ligament assessment) and perform Elson’s test to evaluate for a central slip (see video link below).
- Check for rotational finger dislocations by having patient make a fist and observe for overlapping of phalanges (scissoring).
- Thorough neurovascular exam, with comparison to uninjured hand.
- Capillary refill ≤ 2 seconds.
- Allen test.
- Median nerve injury is common sequalae of volar lunate dislocation into carpal tunnel.
- Visual inspection for open wounds, deformity, discoloration, swelling and atrophy.
Video: Hand Physical Exam [8]
Video: Elson’s Test [10]
- Imaging:
- Diagnosis should be made using X-ray anteroposterior (AP), lateral and oblique views.



Recommended Treatment
- Pain Management:
- Provide via digit nerve, metacarpal or wrist blocks [2] [12] [13](see videos below).
- Video: Peripheral Nerve Blocks for Hand Procedures | NEJM – YouTube
- Video: Single Injection Volar Digital Block – YouTube
- Video: Metacarpal block (youtube.com)
- CMC Dislocation: [6] [7] [14] [15]
- Post reduction stability is most important factor, most require surgery.
- Thumb CMC dislocation treatment, closed reduction is possible (little agreement in literature).
- Metacarpal 2-5, traction of digit with pressure force applied to deformity at base of metacarpal. Cast immobilization for 6 weeks with 70-90° MCP joint flexion, slight flexion of PIP and DIP, and mild wrist extension (i.e., radial or ulnar gutter cast). Schedule follow up X-ray or orthopedic consultation to confirm reduction stability. Loss of reduction is an indication for surgery.
- MCP Dislocation: [5]
- Stabilize the proximal phalanx while applying axial traction to distal phalanges with relocating pressure of the phalangeal base to guide finger back into position.
- Multiple attempts should not be made as this may indicate volar plate involvement requiring surgery.
- Splint with wrist in 30° extension, MCP in 30°-60° flexion, duration 3-6 weeks. Following splint removal, use finger buddy taping 2-3 weeks.
- PIP Dislocation: [5]
- Dorsal dislocation: with one hand apply slight extension and longitudinal traction, with other hand apply pressure to dorsal aspect of proximal phalanx to relocate the dislocated finger.
- Volar dislocation: Apply traction while PIP and MCP are held in slight flexion
- Lateral dislocation: Hold wrist in extension, MCP in flexion and rotate the middle phalanx back into position.
- Apply an extension splint for up 6 weeks. Can introduce buddy taping sooner to reduce edema and allow for earlier rehabilitation.
- DIP Dislocation: [5]
- Reduce dislocation by stabilizing middle phalanx and applying traction.
- Splint DIP in 10°-20° flexion for 2-3 weeks.
Criteria For Hospital Admission
- Other serious injuries related to trauma.
- Unstable patient.
- Infection.
- Surgery.
Criteria For Transfer To Another Facility
- Surgery required, cannot be performed at current facility.
- Current facility unable to manage patient with other trauma related injuries.
Criteria For Close Observation And/or Consult
Indications for Surgery:
- CMC Dislocations: joint stability concern, ligamentous or other soft tissue damage, loss of reduction on follow-up X-ray. [6] [7]
- MCP Dislocations: non-reducible dislocation with high likelihood of volar plate involvement.[5]
- PIP Dislocations: non-reducible dislocation, joint instability or significant ligament, tendon or soft tissue injury. [5]
- DIP Dislocations: irreversible dislocation. [5]
Acute Carpal Tunnel Syndrome following trauma is a surgical emergency.
Criteria For Safe Discharge Home
- If patient admitted for surgery, discharge by admitting service.
- Dislocations reduced in ED: [1]
- Pain adequately managed.
- All associated wounds cleaned and bandaged.
- Antibiotics & Tetanus booster (if required).
- Patient education complete (see patient discharge sheets).
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
The diagnostic process and treatment techniques for MCP, PIP, and DIP dislocations described in this PECS are consistent with literature and available information available online.
For CMC dislocations, the evidence presented in this PECS is Low as these injuries are rare and there are differences of opinion on treatment, especially for thumb CMC joints.
Related Information
OTHER RELEVANT INFORMATION
Patient Discharge Sheet
Finger, Hand, and Wrist Injuries (HealthLink BC): Finger, Hand, and Wrist Injuries | HealthLink BC
Dislocated Finger: Care Instructions (Alberta): Dislocated Finger: Care Instructions (alberta.ca)
Dislocated Finger in Children: Care Instructions (Alberta): Dislocated Finger in Children: Care Instructions (alberta.ca)
- Hand Anatomy Animated Tutorial – YouTube
- Clinical assessment of hand injuries: physical exam
- Emergency Medicine Cases Podcast, Episode 178: Hand Injuries – Pitfalls in Assessment | Emergency Medicine Cases
- Emergency Medicine Cases Podcast, Episode 179: Hand Injuries – Finger Tip Injuries, Jersey Finger, PIP Dislocations, Metacarpal Fractures, Thumb Injuries, Tendon Lacerations | EM Cases (emergencymedicinecases.com)
Reference List
C. Nickson, “Life in the Fast Lane – Extremity Injuries,” 3 November 2020. [Online]. Available: https://litfl.com/extremity-injuries/.
J. Chandrasoma, K. Harrison, H. Ching, L. Vokach-Brodsky and L. Chu, “Peripheral Nerve Blocks for Hand Procedures,” The New England Journal of Medicine, vol. 379, pp. e(15)1 – e(15)5, 6 September 2018.
T. Bentley, N. Hope and J. Journey, Wrist Dislocation, Treasure Island, Florida: StatPearls, 2023.
K. Schnetzler, “Acute Carpal Tunnel Syndrome,” Journal of the American Academy or Orthopaedic Surgeons, vol. 16, pp. 276-282, May 2008.
M. Taqi and A. Collins, Finger Dislocations, Treasure Island, Florida: StatPearls, 2022
O. I. Feder, J. P. Letzelter and J. H. Hacquebord, “Dorsal Dislocation of the trapezoid with Metacarpal Instability: A Boxing Injury,” Journal of Wrist Surgery, vol. 10, no. 3, pp. 245-248, 2021.
G. Drosos, E. Kayias and K. Tsioros, “”Floating thumb metacarpal” or complete dislocation of the thumb metacarpal. A Case report and review of the literature.,” International Journal of the Care of the Injured, vol. 35, pp. 544-547, 2004
D. M. Distefano and D. A. Sayal, “EP 178 Hand Injuries – Pitfalls in Assessment and Management,” 1 January 2023. [Online]. Available: https://emergencymedicinecases.com/hand-injuries-assessment-management/. [Accessed 27 February 2024].
J. Swartz, R. Donaldson, N. Young, P. O. D. Lin, M. Holtz and C. Kim, “Hand Exam,” 25 October 2023. [Online]. Available: https://wikem.org/wiki/Hand_exam.
M. Hayton, “Elsons Test,” 19 March 2009. [Online]. Available: https://www.youtube.com/watch?v=G9HY0qXWUvE. [Accessed 27 February 2024].
C. Hacking, “Dislocated 2nd DIP joint – importance of orthogonal views,” 18 January 202. [Online]. Available: https://radiopaedia.org/cases/73416. [Accessed 21 April 2024].
P. S. Dalhousie, “Single Injection Volar Digital Block,” 17 February 2015. [Online]. Available: https://www.youtube.com/watch?v=G6jyw7l3bZs. [Accessed 20 April 2024]
P. S. Dalhousie, “Metacarpal block,” 17 February 2015. [Online]. Available: https://www.youtube.com/watch?v=SgFiuyDekcc. [Accessed 20 April 2024].
J. Kim, K. Hussain, D. Higginbotham and A. Tsai, “Management of thumb carpometacarpal joing dislocations: A systematic review.,” Journal of Orthopaedics, pp. 59-63, 2021.
C. Jorgensen and S. Christos, “Carpometacarpal Dislocations with Third Metacarpal Fracture,” Clinical Practice and Cases in Emergency Medicine, vol. 5, no. 4, pp. 488-490, 2021.
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated May 01, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.