Hypernatremia
Metabolic / Endocrine
Context
- Hypernatremia = plasma sodium >145 mmol/L
- Mild = Na+ <150 mmol/L
- Severe = Na+ >158 mmol/L
- Acute hypernatremia mortality ≈50-60%.
- More common in the elderly, children, hospitalized patients, and patients that are severely ill.
- Hypernatremia is usually caused by limited access to water or an impaired thirst. mechanism, and less commonly by arginine vasopressindeficiency or resistance (formerly diabetes insipidus).
- Manifestations include confusion, neuromuscular excitability, hyperreflexia, seizures, and coma.
- Patients who do not respond to simple rehydration or in whom there is no obvious cause may need assessment of urine volume and osmolality, particularly after water deprivation.
- Replace intravascular volume and free water orally or intravenously at a rate dictated by how acutely (< 24 hour) or chronically the hypernatremia has developed, while watching other serum electrolyte levels (especially potassium and bicarbonate) as well.
Diagnostic Process
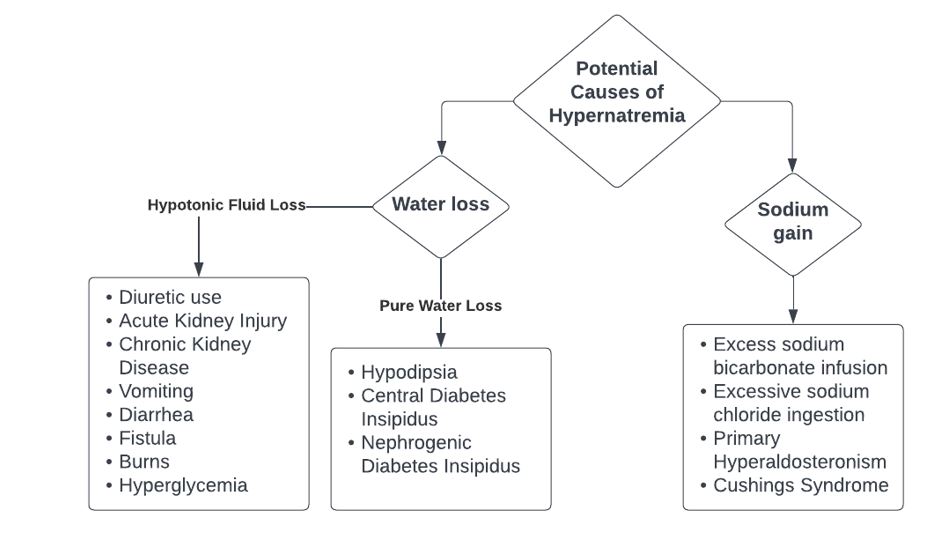
Figure 1: Diagnostic approach to determining underlying cause of hypernatremia.
- Definitions
- Acute hypernatremia occurs within <48 hours.
- Chronic hypernatremia occurs within >48 hours.
- Common conditions associated with hypernatremia:
- Infection (sepsis, pneumonia)
- Trauma
- Intoxication
- Symptoms are more severe with acute hypernatremia.
- Most common symptoms: somnolence, disorientation, falls, severe fatigue, agitation, coma, seizure.
- Symptoms in infants: hyperpnea, muscle weakness, restlessness, insomnia, high-pitched characteristic cry, coma, and lethargy.
- Symptoms in the elderly tend to present after Na+ exceeds 160 mmol/L.
- Review whether patient is taking diuretic medications (which can lead to a hypovolemic & hypernatremic state).
Recommended Treatment
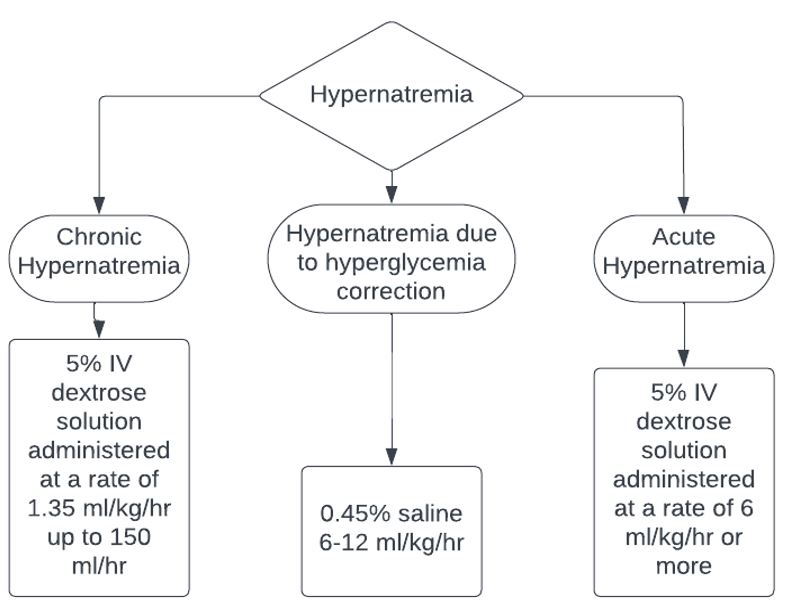
Figure 2: Treatment overview of hypernatremia based on duration.
- Main treatment goals:
- Restore serum sodium to 145 mEq/l.
- Treat any underlying etiology.
- Initial treatment during the first 24 hours and correction of hypernatremia may be inadequate with little decrease in serum sodium.
- Monitor Na+ every 1-3 hours to ensure correction speed is not too fast or slow (see below).
- Chronic hypernatremia
- Administer 5% IV dextrose solution at a rate of 1.35 ml/hr/kg body weight up to a maximum of 150 ml/hr.
- Approximately 100 ml/hr for a 70 kg patient.
- Administer normal saline if patient is hypovolemic.
- May also correct with oral hydration in children with gastroenteritis.
- Administer 5% IV dextrose solution at a rate of 1.35 ml/hr/kg body weight up to a maximum of 150 ml/hr.
- The correction rate for chronic hypernatremia is up to 0.5 mEq/L per hr
- Reduce at a rate of less than 8-10mEq/l/day to avoid consequences from rapid correction.
- Acute hypernatremia
- Administer 5% IV dextrose solution at a rate of 6 ml/hr/kg body weight or more.
- Approximately 420 ml/hr for a 70 kg patient.
- Once sodium reaches 145 mEq/L, reduce infusion rate to 1ml/hr/kg until sodium reaches 140 mEq/L.
- Administer 5% IV dextrose solution at a rate of 6 ml/hr/kg body weight or more.
- The correction rate for acute hypernatremia can be up to 8 mEq/L per hr.
- Goal is to lower sodium levels rapidly in the first few hours and restore normal sodium levels within 24 hours.
- Slow down rate of infusion or use 2.5% IV dextrose solution if risk of hyperglycemia.
- In patients with co-occurring acute kidney injury, consider hemodialysis.
- Hypernatremia due to hyperglycemia correction.
- 45% saline 6-12 ml/kg/hr.
- If < age 40 year old patient treat as chronic hypernatremia.
- If > 40 year old patient treat as acute hypernatremia.
- If patients have hypovolemia or hypokalemia:
- Use hypotonic IV solutions with sodium or potassium simultaneously.
- This will change amount of free water given.
- e.g., If half saline used, replete at a rate of 2.7mL/hr/kg body weight instead of 1.35 mL/hr/kg body weight for chronic hypernatremia.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Although studies exist that outline approaches to hypernatremia, there remains a gap in consensus regarding best treatment practices. There is variation in treatment approaches, and more research is needed to understand the effect of existing recommendations.
Related Information
OTHER RELEVANT INFORMATION
Reference List
Sterns RH, Hoorn EJ. Treatment of hypernatremia [Internet]. 2023 [cited 2024 Jan 1]. Available from: https://www.uptodate.com/contents/treatment-of-hypernatremia-in-adults
Liamis G, Filippatos TD, Elisaf MS. Evaluation and treatment of Hypernatremia: A practical guide for physicians. Postgraduate Medicine. 2016;128(3):299–306. doi:10.1080/00325481.2016.1147322
Adrogué HJ, Madias NE. Hypernatremia. New England Journal of Medicine. 2000;342(20):1493–9. doi:10.1056/nejm200005183422006
Qian Q. Hypernatremia. Clinical Journal of the American Society of Nephrology. 2019;14(3):432–4. doi:10.2215/cjn.12141018
Ravioli S, Rohn V, Lindner G. Hypernatremia at presentation to the Emergency Department: A case series. Internal and Emergency Medicine. 2022;17(8):2323–8. doi:10.1007/s11739-022-03097-4
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jun 04, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.