Intravenous Regional Anesthesia (Bier Block)
Orthopedic, Toxicology, Trauma
First 5 Minutes
- Ensure monitoring attached and resuscitation equipment ready.
- While Local anesthetic systemic toxicity (LAST) is uncommon with the doses described with this technique, a refresher on risk factors is warranted. These include renal/hepatic dysfunction, ischemic heart disease, cardiac conduction abnormalities, extremely young (<4 months) or old (>79 years) patients, pregnancy.
- Complications of LAST include cardiac arrest, seizures, hypotension, arrhythmias and death.
Context
- Indications:
- Local anesthesia for procedures occurring on the hand or forearm. In some cases it can also be performed below the knee for distal lower leg procedures.
- This technique may be useful in situations where help is not available and general anesthesia may be risky, however the risk of LAST may outweigh this.
- Benefits: simplicity, low technological needs (e.g., Ultrasound), avoidance of general anesthesia, creation of a bloodless field, faster recovery time, decreased complications compared to general anesthesia.
- Contraindications:
- Local anesthesia (LA) allergy, known DVT, open wounds, severe hypertension >175mmHg systolic, Raynauds, Sickle cell disease, crush injuries, young child, unreliable tourniquet.
- DO NOT use bupivacaine for this procedure due to increased cardiac toxicity.
- Considerations:
- Would performance of alternative local anesthesia be better suited to this procedure?
- If tourniquet pain develops, the distal tourniquet may be inflated and the proximal deflated.
- Once LA is injected, the cuff should remain inflated for at least 20 minutes to decrease LAST risk.
- Adverse outcomes have been reported in 1.6% of patients, mostly consisting of minor symptoms of LAST (transient tinnitus, mild bradycardia, tinnitus)(5).
- Practitioners performing IVRA should be comfortable treating LAST.
Search media [Internet]. Wikimedia.org. [cited 2023 Nov 28]. Available from: https://commons.wikimedia.org/w/index.php?search=bier+block&title=Special:MediaSearch&go=Go&type=image
Recommended Treatment
TECHNIQUE: Adapted from the stat-pearls article https://www.ncbi.nlm.nih.gov/books/NBK430760/
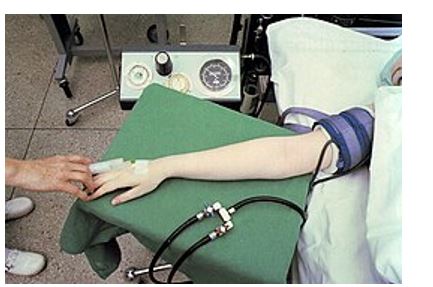
- Insert two IV’s, one in the forearm as close as possible to the site of the procedure, one in the opposite arm for fluid resuscitation and systemic medications as needed.
- Elevate the extremity for 2-3 minutes for passive drainage.
- Place a roll of gauze in the patient’s hand for decreased discomfort from the Esmarch bandage.
- After ensuring the double cuffed tourniquet is in place, apply an Esmarch bandage to the extremity to actively exsanguinate. For a technique see following video. https://vimeo.com/548413479
- Inflate the distal cuff of the tourniquet to 250mmHg or 100mmHg above systolic BP, followed by the proximal tourniquet.
- Tourniquet is inflated for at least 30 minutes and at most 60 minutes.
- Ensure that brachial and radial pulses are not palpable.
- Release the distal cuff and remove the Esmarch bandage.
- Inject local anesthetic into the IV slowly to avoid spread past the tourniquet. Typical dosing depends on the placement of the tourniquet. Placement above the elbow dosing is generally 40ml of 0.5% lidocaine. If possible to place the tourniquet below the elbow this is preferable due to the reduced lidocaine dosing needed, approximately 30mL of 0.5% lidocaine. (The maximum dose is 3ml/kg of lidocaine. It should be preservative free and WITHOUT epinephrine.)
- Remove the IV.
- Once onset of regional anesthesia is confirmed, the procedure may be performed.
- The proximal cuff may be deflated after 30 minutes and once the procedure is completed.
Criteria For Close Observation And/or Consult
- It is very important that those doing this procedure know how to recognize LAST and have the drugs and ability to treat it rapidly and monitor patients for 30 minutes after procedure for signs of LAST.
- LAST CNS and cardiovascular signs and symptoms include tinnitus, dysarthria, numbness, agitation, seizure, ALOC, respiratory arrest, systemic shock, bradycardia, ventricular arrhythmia.
- LAST Treatment includes oxygenation to prevent hypoxia which can exacerbate complications, benzodiazepines for seizures. The mainstay of treatment is lipid emulsion therapy with intralipid. Give Intralipid 20% IV at a dose of 1.5 mL/kg (maximum: 100 mL) over 1 to 3 minutes, followed by a 0.25 mL/kg/minute infusion (maximum: 200 to 250 mL over 15 to 20 minutes). Repeat bolus as needed for ongoing hemodynamic instability.
- For cardiac issues follow ACLS guidelines with some adjustments. Epinephrine can be administered at smaller doses (less than 1mcg/kg). Avoid vasopressin for risk of pulmonary hemorrhage. Avoid Beta blockers or Ca channel blockers. For ventricular arrhythmia use amiodarone.
- Otherwise, based on the issue requiring the procedure.
Criteria For Safe Discharge Home
- Completion of required procedure.
- No S/S of LAST.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Expert opinion and experience only.
Related Information
OTHER RELEVANT INFORMATION
Intercostal nerve block: https://emergencycarebc.ca/clinical_resource/intercostal-nerve-block/
Upper extremity nerve block: https://www.uptodate.com/contents/upper-extremity-nerve-blocks-techniques?search=bier%20block&source=search_result&selectedTitle=1~50&usage_type=default&display_rank=1#H1821229416
Reference List
Kraus GP, Rondeau B, Fitzgerald BM. Bier Block. StatPearls Publishing; 2023.
Vaughn N, Rajan N, Darowish M. Intravenous regional anesthesia using a forearm tourniquet: A safe and effective technique for outpatient hand procedures. Hand (N Y) [Internet]. 2020;15(3):353–9. Available from: http://dx.doi.org/10.1177/1558944718812190
Dekoninck V, Hoydonckx Y, Van de Velde M, Ory J-P, Dubois J, Jamaer L, et al. The analgesic efficacy of intravenous regional anesthesia with a forearm versus conventional upper arm tourniquet: a systematic review. BMC Anesthesiol [Internet]. 2018 [cited 2023 Nov 28];18(1). Available from: http://dx.doi.org/10.1186/s12871-018-0550-4
Fauteux-Lamarre E, Burstein B, Cheng A, Bretholz A. Reduced length of stay and adverse events using Bier block for forearm fracture reduction in the pediatric emergency department. Pediatr Emerg Care [Internet]. 2019;35(1):58–62. Available from: http://dx.doi.org/10.1097/pec.0000000000000963
Brown EM, McGriff JT, Malinowski RW. Intravenous regional anaesthesia (Bier block): review of 20 years’ experience. Can J Anaesth [Internet]. 1989;36(3 Pt 1):307–10. Available from: http://dx.doi.org/10.1007/BF03010770
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jan 04, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.