Irritable Bowel Syndrome
Gastrointestinal
First 5 Minutes
Red flags for pathology in patients with irritable bowel syndrome (IBS):
- GI bleeding (e.g., melena and rectal bleeding).
- Unexplained weight loss.
- Progressive abdominal pain.
- Onset after age 50.
- Nocturnal diarrhea (unusual in IBS).
- Iron deficiency anemia, elevated CRP or fecal calprotectin/lactoferrin.
- Family history of inflammatory bowel disease (IBD) or colorectal cancer.
Causes of acute abdominal pain should be ruled out – AVOID premature closure bias.
Context
IBS is common: abdominal pain and altered bowel patterns (diarrhea, constipation, or both).
The prevalence of IBS in Canada is ~12%.
IBS is more common in:
- Women aged 20-40.
- Those with psychiatric disorders.
- Those with functional somatic syndromes (e.g., chronic fatigue, fibromyalgia).
- Individuals under the age of 50.
IBS is associated with visceral hypersensitivity and abnormal motility.
Diagnostic Process
- Diagnosis is clinical and relies on patient self-reporting of symptoms as well as ruling out other causes.
- Consider red flags.
- Patients may report acute enteric infection prior to onset of IBS symptoms.
- Assess family history of celiac disease.
- Differential diagnosis:
- Celiac disease.
- Inflammatory Bowel Disease (IBD).
- Colorectal cancer.
- Microscopic colitis.
- Small intestinal bacterial overgrowth (SIBO).
- There are different subcategories of IBS:
- IBS with diarrhea
- IBS with constipation
- IBS with mixed stool pattern, and
- IBS unclassified.
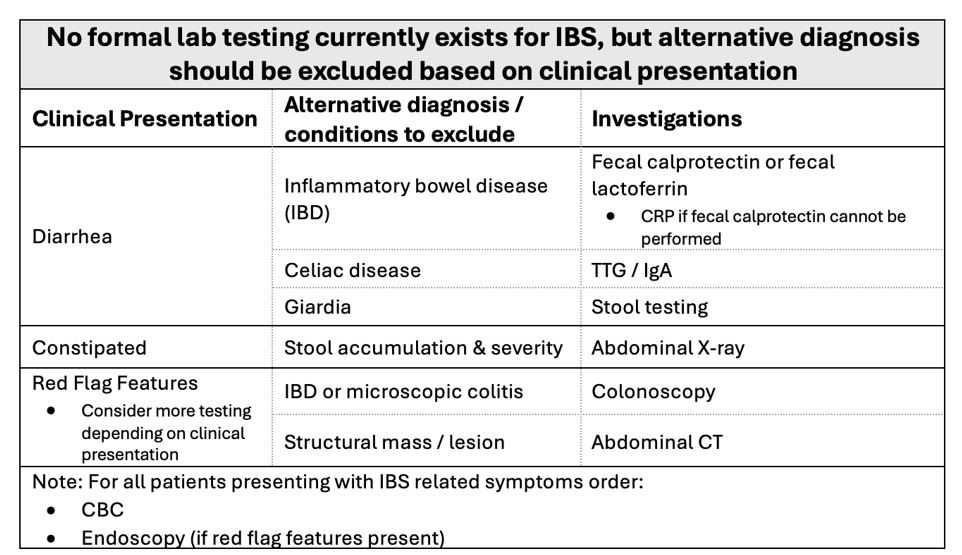
Table 2: Lab and imaging investigations for disorders related to IBS.
Recommended Treatment
Continuity of care and the physician-patient relationship are considered critical in the management of IBS, so consider referral to a longitudinal physician.
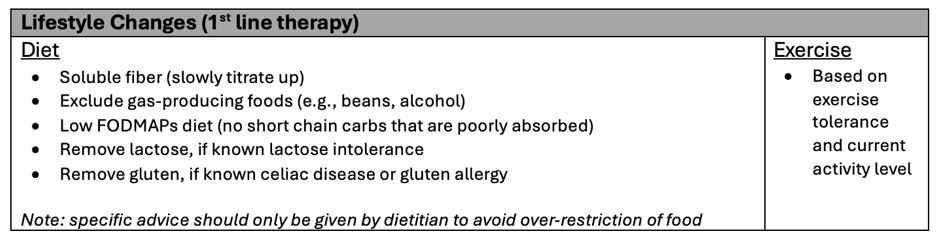
Table 3: Non-pharmacological therapy for IBS.
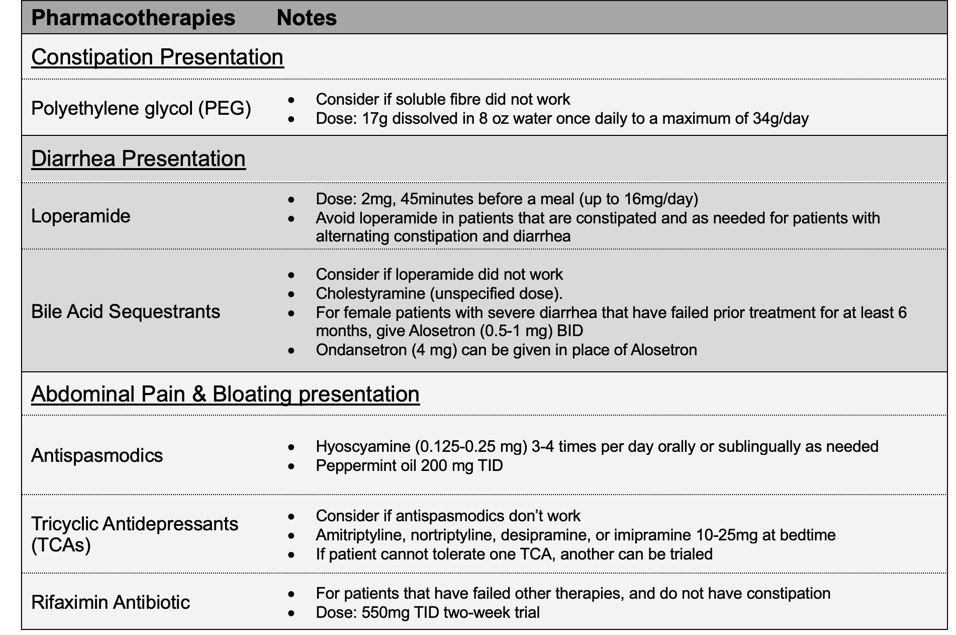
Table 4: Pharmacological therapy option for IBS.
For patients that continue to have refractory symptoms, consider referral for behavioural modification (e.g., cognitive behavioural therapy, gut-directed hypnotherapy, relaxation therapy, dynamic psychotherapy) or use of anxiolytics for less than two weeks to reduce anxiety if present (e.g., benzodiazepines or gabapentin).
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Consensus does not exist on investigations to order and therapies that should be considered in the treatment of IBS – low
Medication dosages including bile acid sequestrants, TCA’s for the purposes of IBS – low
Efficacy of treatments – low
Related Information
OTHER RELEVANT INFORMATION
Reference List
Wald A. Treatment of irritable bowel syndrome in adults [Internet]. 2023 [cited 2024 Jan 19]. Available from: https://www.uptodate.com/contents/treatment-of-irritable-bowel-syndrome-in-adults?search=irritable+bowel+syndrome+treatment&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H1579095076
Wald A. Clinical manifestations and diagnosis of irritable bowel syndrome in adults [Internet]. 2023 [cited 2024 Jan 19]. Available from: https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-irritable-bowel-syndrome-in-adults?search=irritable+bowel+syndrome&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2#H2525434223
Ford AC, Sperber AD, Corsetti M, Camilleri M. Irritable bowel syndrome. The Lancet. 2020;396(10263):1675–88. doi:10.1016/s0140-6736(20)31548-8
Moayyedi P, Andrews CN, MacQueen G, Korownyk C, Marsiglio M, Graff L, et al. Canadian Association of Gastroenterology Clinical Practice Guideline for the management of Irritable Bowel Syndrome (IBS). Journal of the Canadian Association of Gastroenterology. 2019;2(1):6–29. doi:10.1093/jcag/gwy071
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jun 04, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.