Menorrhagia –Diagnosis and Treatment
Metabolic / Endocrine, Obstetrics and Gynecology
Context
Menorrhagia, or prolonged or excessive uterine bleeding, can have a significant impact on quality of life.
- 75% of hysterectomies relate to fibroids/menorrhagia worldwide.
- ~1 in 20 women between 30-49 years of age will present with heavy menstruation each year.
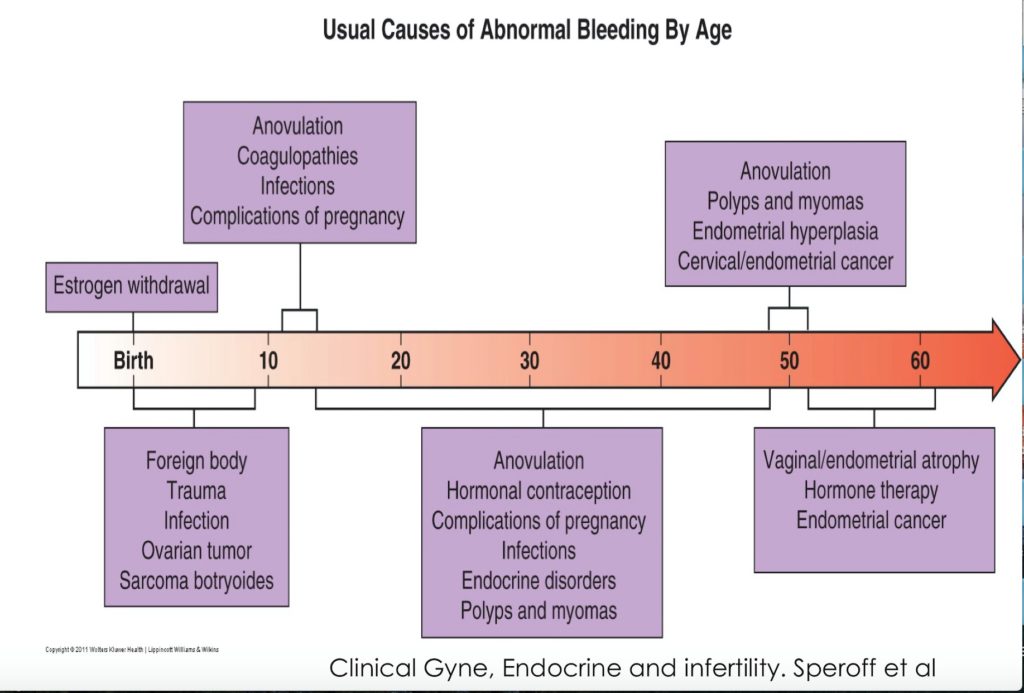
- Menstrual irregularities most frequent in adolescence and perimenopause.
- Clinical starting point: rule out pregnancy.
Approach in non-pregnant women of reproductive age:
-
- Rapid assessment of clinical picture and hemodynamic stability.
- Determine etiology.
- Same for acute and chronic bleeding.
- Choose appropriate treatment.
Diagnostic Process
Presentation:
-
- Menstrual bleeding that lasts >7 days.
- Heavy bleeding (>80cc of blood loss/cycle – hard to quantify clinically).
- Needing to change pad or tampon after <2hrs.
- Passing clots larger than the size of a quarter.
- Bleeding that significantly affects the quality of life.
- Some patients may have anemia, fatigue, and weakness.
- Anovulatory cycles are a common cause of menorrhagia:
- More common at menarche and menopause and with PCOS and obesity.
- Symptoms classically include: hx of irregular periods, late period, and/or mid-cycle spotting.
- Note: spotting can also be a symptom of implantation bleedingin early pregnancy and with normal ovulation.
- Changes to PMS symptoms due to different hormone levels.
Causes of anovulation:
-
-
- Severe changes to diet and/or exercise.
- Prolonged stress.
- Disruption to routine.
- Existing medical conditions such as PCOS.
- Menopause.
-
Differential Diagnosis (PALM-COEIN)
-
- Structural (PALM) and non-structural (COEIN) causes:
- Structural:
- Polyp: 16% of cases*.
- Adenomyosis: 5%.
- Leiomyoma: 12%*.
- Malignancy and hyperplasia: 2%.
- Non-structural:
- Coagulopathy: 1%.
- Ovulatory dysfunction: 58%*.
- Endometrial: 2%.
- Iatrogenic: 2%.
- Not yet classified 1%.
- Structural:
- Structural (PALM) and non-structural (COEIN) causes:
Physical Exam:
-
- Initial assessment à signs of hypovolemia and anemia?
- Confirm bleeding is uterine
- Rule out any trauma/abnormality to the genital tract, vagina or cervix.
- Uterine enlargement or irregularity à potential structural cause
- Consider initiating treatment if low risk of malignancy, fibroids, uterine or histological abnormality or adenomyosis
Investigations and Imaging:
-
- General laboratory Tests
- All patients:
- CBC, pregnancy test, blood type and cross match if unstable or symptomatic anemia.
- Heavy bleeding from menarche / family history of bleeding disorders:
- INR, PTT, Fibrinogen, von Willebrand factor antigen, Factor VIII
- Depending on clinical picture, can also consider:
- TSH, serum Fe, total iron binding capacity, ferritin, liver function tests, infection (chlamydia trachomatis).
- Structural Entities:
- Imaging:
- 1st line: ultrasound (often transvaginal).
- Endometrial Biopsy Indications:
- >40 yrs of age.
- Any risk factor for endometrial cancer: >90kg, nulliparity, Polycystic Ovary Syndrome (PCOS), diabetes, hereditary nonpolyposis colorectal cancer (HNPCC – also known as Lynch Syndrome).
- Failure of medical treatment.
- Significant intermenstrual bleeding (IMB).
- Woman of any age with past anovulatory cycles—patient describes irregular or infrequent periods on hx.
- Postmenopausal women with Endometrial Thickening >4mm on ultrasound.
- Imaging:
- All patients:
- General laboratory Tests
Recommended Treatment
Considerations
Clinical stability, suspected etiology, comorbidities and wishes for future fertility.
- Menorrhagia may present with significant anemia and require emergent care.
Emergency Dept
- NSAIDsare the first-line medical therapy in ovulatory menorrhagia.
- Average reduction of 20-46% in menstrual blood flow.
- Reduce prostaglandin levels by inhibiting cyclooxygenase (higher PG levels in endometrium of pts who have menorrhagia cf. non-menorrhagia).
- 5 days of the entire cycle, limiting stomach upset from NSAIDs.
- Food for mild bleeding and pain.
- Tranexamic acid.
- Better than NSAIDS.
- Blocks lysine binding on plasminogen and prevents fibrin degradation.
- 1 g PO QID x 4/7.
- Adverse effects: N, V, D, Venous Thromboembolism (odds ratio for VTE = 3.20 (95% CI 0.65–15.78).
- Provera.
- Progestin (medroxyprogesterone) is the most frequently prescribed medicine for menorrhagia (especially anovulatory).
- Significant reduction in menstrual blood flow when used alone.
- Works as an antiestrogen by minimizing the effects of estrogen on target cells, thereby maintaining the endometrium in a state of down-regulation.
- Adverse effects: weight gain, headaches, edema, and depression.
*Refer to gynecology if treatments are unsuccessful at controlling symptoms, symptoms are severe, or a large structural defect is identified.
Surgical Management
-
- Endometrial Ablation.
- Similar patient satisfaction, less anesthetic, and fewer risks of complication than hysteroscopic ablation.
- Hysteroscopic myomectomy: for bleeding secondary to fibroids.
- Hysterectomy = definitive treatment for abnormal uterine bleeding.
- Endometrial Ablation.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
- Recommendations based on systematic reviews and three main clinical guidelines: Moderate
Related Information
OTHER RELEVANT INFORMATION
Reference List
Management of acute abnormal uterine bleeding in nonpregnant reproductive-aged women.
Obstet Gynecol. 2013; 121: 891-896.
American College of Obstetricians and GynecologistsACOG.Clinical gynecologic endocrinology and infertility
Fritz MA, Speroff L. . 2012.
Publisher: Philadelphia : Lippincott Williams & Wilkins,Women presenting to an emergency facility with abnormal uterine bleeding: patient characteristics and prevalence of anemia.
Matteson KA, Raker CA, Pinto SB, Scott DM, Frishman GN. 2012;57(1-2):17-25.
J Reprod Med.The two FIGO systems for normal and abnormal uterine bleeding symptoms and classification of causes of abnormal uterine bleeding in the reproductive years
Munro MG, Critchley HO, Fraser IS, et al. :2018; 143(3): 393-408. 2018 revisions.
J. Gynecol.Heavy menstrual bleeding: assessment and management.
National Guideline Alliance. 2018.
National Institute for Health and Care ExcellenceAbnormal uterine bleeding in pre-menopausal women.
Singh S, Best C, Dunn S, et al. 2013; 35(5): 473-475.
J Obstet Gynaecol Can.
Journal of Obstetrics and Gynaecology CanadaPrevalence of abnormal uterine bleeding according to new International Federation of Gynecology and Obstetrics classification in Chinese women of reproductive age: A cross-sectional study.
Sun Y, Wang Y, Mao L, Wen J, Bai W. 2018;97(31).
Medicine® journal (Online).
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Apr 04, 2021
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.