Missed OAT Doses
Analgesia / Sedation, Special Populations, Substance Use
First 5 Minutes
- Quickly recognize and address opioid withdrawal syndrome.
- Identify patients on opioid agonist therapy and inquire about missed doses.
- Deliver any missed doses expeditiously to help patient stay engaged in care.
- System level: Ensure your ED has ward stock & workflows to deliver missed doses quickly.
Context
- Oral opioid agonist therapies (OAT), including buprenorphine/naloxone, methadone, and slow-release oral morphine (SROM), are evidence-based treatments for opioid use disorder (OUD) that reduce incidence of opioid poisoning, HIV/HCV transmission, and all-cause mortality.
- OAT discontinuation or interruption is associated with a higher risk of fatal overdose.
- The ED is a common point of contact with healthcare for individuals with OUD, and thus represents a critical opportunity to support OAT engagement and continuation.
Recommended Treatment
General Guidance
- Provide missed dose if long ED stay anticipated or logistical barriers to getting to pharmacy or delivery location on time.
- If the patient is not in opioid withdrawal and has a medical issue that is easy to resolve fully and quickly during business hours, facilitating transport to their OAT dispensing pharmacy may benefit continuity of care. In all other cases, OAT doses should be provided in the ED.
- Consult your on-call addiction specialist or the BCCSU 24/7 Addiction Medicine Clinician Support Line (778-945-7619) for:
- iOAT (injectable OAT).
- Alternative dosing schedules (i.e., split dosing).
- Other complicating factors (i.e., acute medical illness, concurrent intoxication or withdrawal).
- OAT does not equal pain control but can assist in more effective pain management. If someone presents with a missed dose and a wrist fracture, provide OAT and appropriate analgesia.
- For all missed doses, discuss reasons for missed dose and arrange follow-up with prescriber for review with goal of supporting patient for better OAT retention.
- Notify community pharmacy of any dose provided in the ED.
Calculating Missed Doses
- Do not count day of ED presentation.
- Review Pharmanet profile and use in conjunction with patient provided history.
- Caution: Pharmacies will often list today’s dose as “dispensed” when it has been prepared but not dispensed. Often not “reversed” until following day”.
- Contact pharmacies directly if during opening hours to confirm if dose dispensed and notify of dose provided in the ED to prevent double dosing.
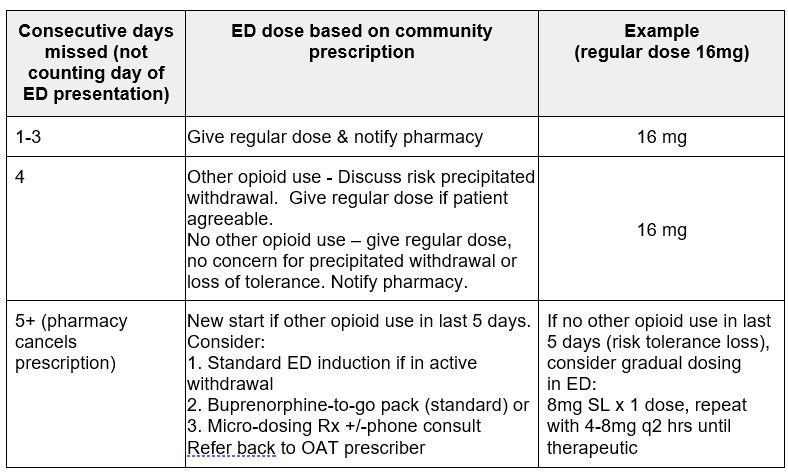
Buprenorphine / Naloxone (Suboxone)
Missed Dose Protocol
- Ask whether patient has resumed using full opioid agonists. This will affect care for ≥ 4 days missed (see table).
- Often prescribed as weekly dispensed, and may not have any witnessed doses – therefore confirm last dose with patient.
Missed Extended-Release Subcutaneous Buprenorphine (Sublocade) Doses
- Up to 2 weeks delay in monthly injection acceptable. Patient should be directed to community provider or dose can be provided in ED.
- If over 2 weeks delay in monthly injection, re-induction warranted.
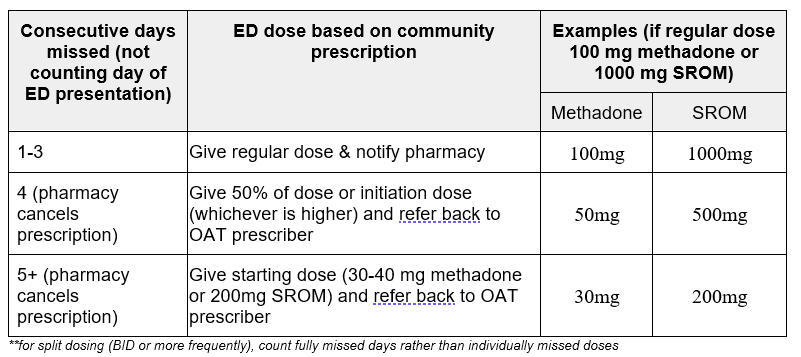
Methadone & Slow Release Oral Morphine (SROM or Kadian)
Missed Dose Protocol
- BCCSU’s guideline on missed doses endorses resumption of patient’s usual dose for up to 3 consecutive missed once-daily doses.
Discharge Planning
- Ensure adequate follow-up, especially if new prescription needed. Call local addiction team/provider or BCCSU 24/7 support line for bridging prescription as indicated.
- Consider social work, peer navigator & outreach team support to address barriers that led to missed doses, including transport to prescriber and/or pharmacy
- Offer take-home naloxone and safer use supplies.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
There is high quality evidence that a) OAT discontinuation leads to increased mortality and other negative outcomes for people who use opioids and that b) ED patients with opioid poisoning have elevated 1-year mortality risk. While it makes intuitive sense to provide OAT in the ED, there is no direct evidence that OAT continuation in the ED improves outcomes.
Related Information
OTHER RELEVANT INFORMATION
Reference List
British Columbia Centre on Substance Use and B.C. Ministry of Health. A Guideline for the Clinical Management of Opioid Use Disorder – 2023 Update. British Columbia Centre on Substance Use; 2023. Accessed June 1, 2024. https://www.bccsu.ca/wp-content/uploads/2023/12/BC-OUD-Treatment-Guideline_2023-Update.pdf
Pearce L, Min JE, Piske M, et al. Opioid agonist treatment and risk of mortality during opioid overdose public health emergency: population based retrospective cohort study. BMJ. 2020;368:m772. https://doi.org/10.1136/bmj.m772
Krebs E, Homayra F, Min JE, et al. Characterizing opioid agonist treatment discontinuation trends in British Columbia, Canada, 2012-2018. Drug Alcohol Depend. 2021;225:108799. doi: 10.1016/j.drugalcdep.2021.108799.
Moe J, Chong M, Zhao B, et al. Death after emergency department visits for opioid overdose in British Columbia: a retrospective cohort analysis. CMAJ Open. 2021;9(1):E242-E251. https://doi.org/10.9778/cmajo.20200169
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Aug 21, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.