Neonatal Jaundice
Pediatrics
First 5 Minutes
All unwell jaundiced infants require early evaluation:
Red flags:
- Known family history of significant hemolytic disease.
- Vomiting.
- Lethargy.
- Poor feeding.
- Fever.
- High-pitched cry.
- Dark urine.
- Light stools.
Context
- Neonatal jaundice is a very common condition worldwide, occurring in up to 60% of term and 80% of preterm newborns in the first week of life with serum bilirubin levels >5 mg/dL (>85.5 µmol/L).
- Hyperbilirubinemia tends to occur in the first week after birth due to normal physiologic changes and is often harmless.
- Common cause of newborn readmission to hospital and emergency visits, especially in the first two weeks of life.
- Seen more commonly among preterm newborns.
The breakdown of hemoglobin in red blood cells releases unconjugated bilirubin (indirect bilirubin) into the bloodstream, which is then converted to conjugated bilirubin (direct bilirubin) in the liver.
- Indirect bilirubin is lipid-soluble and can cross the blood-brain barrier, thus making it a neurotoxic substance (kernicterus risk).
- Direct bilirubin is more easily excreted (if elevated, this is always pathological, requiring further investigation).
In newborns, excessive levels of indirect bilirubin in the blood can lead to encephalopathy (kernicterus).
- Kernicterus is a life-threatening infiltration of bilirubin into the brain, depositing in basal ganglia and brainstem nuclei.
- Penetration of the blood-brain barrier is more likely when bilirubin >25–30 mg/dL (425-510 µmol/L).
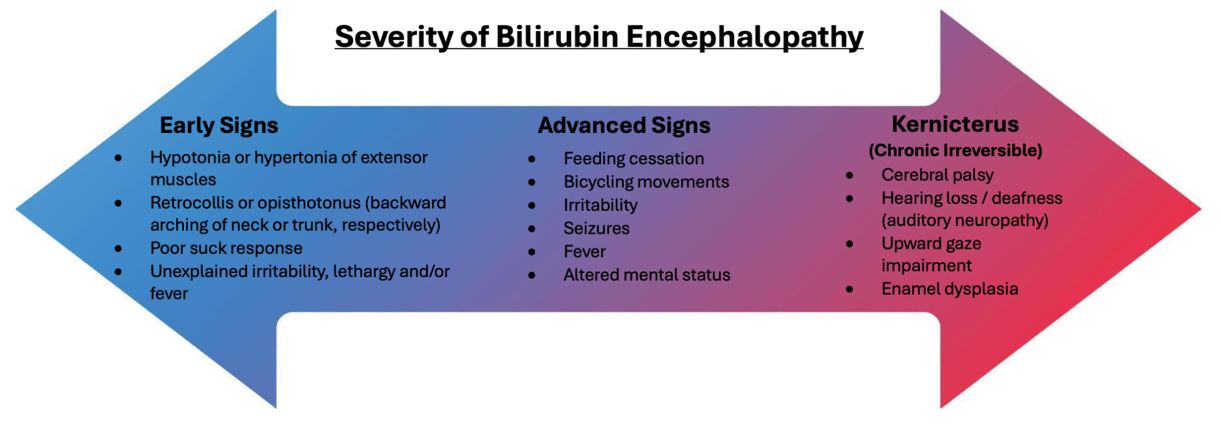
Figure 1: Signs of Bilirubin Encephalopathy.
Diagnostic Process
The main causes of jaundice in neonates tend to be due to elevated indirect bilirubin, and include:
- Increase in hemolysis (increased RBC breakdown).
- Delayed maturation or inhibition of liver conjugation enzymes.
- Interference with liver uptake of indirect bilirubin.
Indirect bilirubin elevation = physiologic or pathologic.
Direct bilirubin elevation = pathologic.
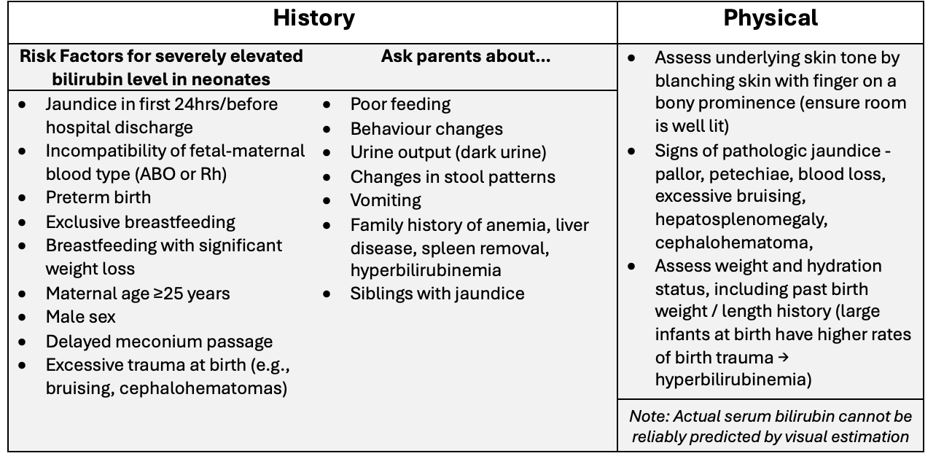
Table 1. Initial Assessment Tips for Jaundice in Newborn.
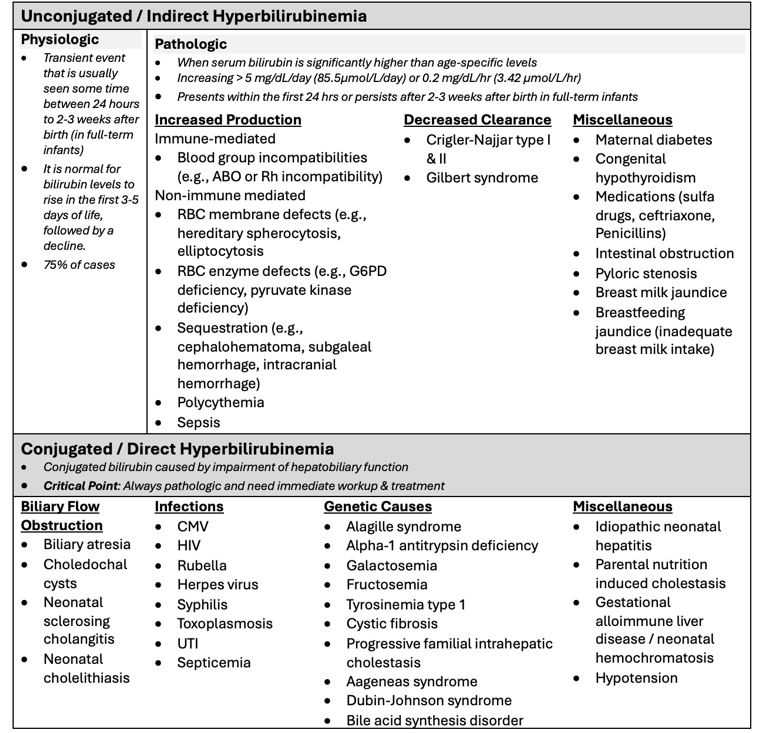
Table 2. Etiologies of Jaundice in Newborn.
Evaluation:
- Newborns may be observed if they: are full-term, appear clinically well, are asymptomatic, have no warning signs, or have a presentation consistent with physiologic jaundice (Table 1).
- For jaundiced infants, order serum bilirubin and hemoglobin → no further testing needed if normal level in well-appearing, afebrile baby.
- May consider getting a urinalysis and urine culture.
- Investigations for pathologic neonatal jaundice:
- CBC
- Total serum bilirubin (TSB)
- Direct and Indirect Bilirubin
- Direct Coombs’ test
- Blood group testing (maternal and fetal)
- Hemoglobin
- Reticulocyte count
- Liver function test
- Alkaline phosphatase
- Serum albumin
- PTT/INR
- TSH
- Urinalysis
- Full septic work-up (in addition to the above, do a WBC count, chemistry panel, CRP, urine culture, blood culture, and a lumbar puncture)
- TORCH infection panel – for infectious cause workup in direct hyperbilirubinemia.
- Consider abdominal ultrasound to investigate obstructive causes (biliary atresia is most common direct cause).
- If exchange transfusion is anticipated (see Table 3 below), obtain blood type and crossmatch.
- Hemolysis is suspected if there is: reticulocytosis, indirect hyperbilirubinemia, and a peripheral smear consistent with RBC destruction.
Recommended Treatment
Management decisions should be made carefully, with consideration to the benefits and risks of each treatment as well as the neonate’s age, clinical appearance, bilirubin level, etiology, and jaundice onset/timing.
Admit the neonate and consult a neonatologist if:
- They are anemic, hyperbilirubinemia level indicates phototherapy or exchange transfusion treatment, or there is pathologic/conjugated hyperbilirubinemia.
- To find out which serum bilirubin levels phototherapy or exchange transfusion are indicated, see current Canadian Pediatric Society guidelines and nomogram (in-depth review section) as the value is age dependent.
The goal for indirect hyperbilirubinemia is to prevent kernicterus, as this can cause permanent brain injury or even death.
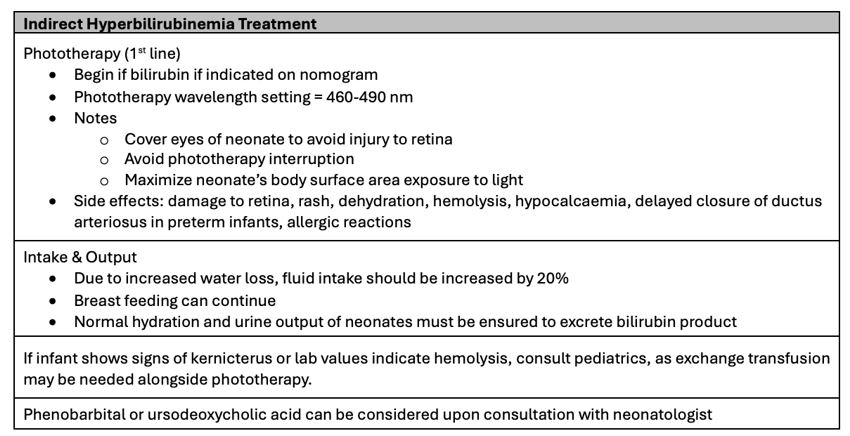
Table 3: Treatment of Indirect Hyperbilirubinemia.
The goal for managing direct hyperbilirubinemia is to immediately identify and treat the underlying cause of a patient’s symptoms:
- Start antibiotics if sepsis or urinary tract infection are suspected as the cause of jaundice.
- If obstruction or biliary atresia suspected, consult Pediatric Surgery regarding hepatic portoenterostomy.
Full-term, afebrile neonates that appear well and have a bilirubin level of low risk (based on nomogram) can be monitored closely and supported conservatively:
- Encourage frequent breastfeeds (8-10 times per 24 hours) and stools to support excretion of bilirubin.
- Administer IV bolus normal saline depending on weight if signs of dehydration.
- It is encouraged to not discontinue breastfeeding.
- Discuss different feeding options (e.g., continued breastfeeding, brief substitution with formula, and supplementing with formula) including their risks and benefits while considering parents’ preference.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Guidelines for intensive phototherapy of infants 35 or more weeks gestation.
Related Information
OTHER RELEVANT INFORMATION
Reference List
Ansong-Assoku B, Shah SD, Adnan M, Ankola PA. Neonatal jaundice – statpearls – NCBI bookshelf [Internet]. 2023 [cited 2024 Jan 27]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532930/
Taylor T, Wheatley M. Jaundice in the Emergency Department: Meeting the Challenges of Diagnosis and Treatment [Internet]. 2018 [cited 2024 Jan 26]. Available from: https://www.ebmedicine.net/topics/hepatic-renal-genitourinary/jaundice-bilirubin
Maisels MJ. Managing the jaundiced newborn: A persistent challenge. Canadian Medical Association Journal. 2014 Nov 10;187(5):335–43. doi:10.1503/cmaj.122117
Colletti JE, Kothari S, Jackson DM, Kilgore KP, Barringer K. An emergency medicine approach to neonatal hyperbilirubinemia. Emergency Medicine Clinics of North America. 2007 Nov 22;25(4):1117–35. doi:10.1016/j.emc.2007.07.007
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jun 04, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.