Non-invasive Ventilation
Critical Care / Resuscitation, Respiratory
First 5 Minutes
Consider in 3 main conditions:
- Acute pulmonary edema associated with heart failure.
- COPD exacerbation.
- Asthma – less evidence for value.
Patients must be able to breathe by themselves as this does not provide mechanical breathing.
Contraindications:
- Need immediate intubation.
- Uncooperative patient – altered mental status, anxiety.
- Risk of aspiration – vomiting, hematemesis.
- Hemodynamic instability.
Context
- Non-invasive ventilation can improve ventilation, oxygenation, and work of breathing leading to improved outcomes and reduced intubation/ventilator use.
- Shorter ICU stays.
Non-invasive ventilation can involve supplementing oxygen with nasal cannulas, oronasal face masks, and helmets.
Some common forms of non-invasive ventilation include:
- Continuous positive airway pressure (CPAP).
- used for acute pulmonary edema, asthma, obstructive sleep apnoea (OSA).
- Bilevel positive airway pressure (BIPAP), inspiratory positive airway pressure (IPAP), and expiratory positive airway pressure (EPAP).
Diagnostic Process
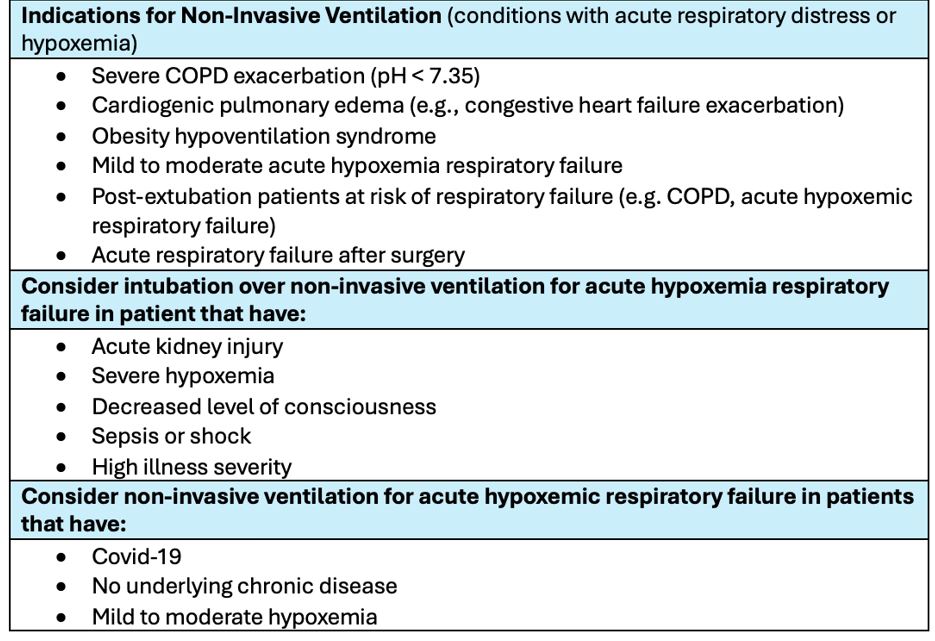
Table 1. Considerations for Non-Invasive Ventilation
Closely monitor respiratory rate, level of consciousness and PaO2 to FIO2 trajectory in case of potential failure.
Recommended Treatment
- Healthcare teams should be experienced with non-invasive respiratory support and ventilation settings for greater utility.
- Treatment for COPD, obesity hypoventilation syndrome, and cardiogenic pulmonary edema should first involve a method of non-invasive ventilation that the team is comfortable in, with early monitoring of signs of failure.
- Considerations in selecting non-invasive ventilation device although most people
- High flow nasal cannula
- More comfortable.
- Can use in prone position.
- Least effective delivery of PEEP.
- Face mask
- More effective delivery of PEEP than high flow nasal cannula.
- Helmet
- Most effective delivery of PEEP.
- Greater tolerance, fewer breaks off device needed.
- Can deliver CPAP without ventilator if in low resource setting.
- May be able to overcome airway closure or auto-PEEP.
- More claustrophobic.
- Challenging to use in prone position.
- Challenging to perform investigations.
- Lengthier transition to intubation.
- Greater learning curve.
- High flow nasal cannula
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Quality of evidence is low considering a lot of inconclusive evidence towards specific conditions remains with gaps in the literature. Future studies are expected to have a large effect in changing recommendations surrounding non-invasive ventilation use.
Related Information
OTHER RELEVANT INFORMATION
- https://oce.ovid.com/article/00003246-201602000-00006/HTML (Acute Simplified Physiology Score II)
- https://link.springer.com/article/10.1007/s00134-016-4601-3 (HACOR Score)
- https://www.uptodate.com/contents/noninvasive-ventilation-in-adults-with-acute-respiratory-failure-benefits-and-contraindications?search=noninvasive%20ventilation&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H96523994
- https://www.uptodate.com/contents/noninvasive-ventilation-in-adults-with-acute-respiratory-failure-practical-aspects-of-initiation?search=noninvasive%20ventilation&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2
- https://www.ebmedicine.net/topics/respiratory/pediatric-noninvasive-ventilation
Reference List
Penuelas O, Frutos-Vivar F, Esteban A. Noninvasive positive-pressure ventilation in acute respiratory failure. Canadian Medical Association Journal. 2007;177(10):1211–8. doi:10.1503/cmaj.060147
Munshi L, Mancebo J, Brochard LJ. Noninvasive respiratory support for adults with acute respiratory failure. New England Journal of Medicine. 2022;387(18):1688–98. doi:10.1056/nejmra2204556
Digby GC, Keenan SP, Parker CM, Sinuff T, Burns KE, Mehta S, et al. Noninvasive ventilation practice patterns for acute respiratory failure in Canadian tertiary care centres: A descriptive analysis. Canadian Respiratory Journal. 2015;22(6):331–40. doi:10.1155/2015/971218
Keenan SP, Sinuff T, Burns KE, Muscedere J, Kutsogiannis J, Mehta S, et al. Clinical practice guidelines for the use of noninvasive positive-pressure ventilation and noninvasive continuous positive airway pressure in the acute care setting. Canadian Medical Association Journal. 2011;183(3). doi:10.1503/cmaj.100071
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated May 21, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.