Pleural Effusion
Cardiovascular, Infections, Inflammatory, Respiratory
First 5 Minutes
- ABCs – ensure adequate oxygenation and ventilation.
- Imaging is typically needed for further evaluation.
- X-ray imaging is a good first choice, but point of care ultrasound can be useful – pneumonia vs. effusion.
- Sick or not sick? Patients with parapneumonic effusions or hemodynamic instability will need prompt initiation of antibiotics and chest tube thoracostomy with (pigtail) drain.
Context
- Excess fluid accumulation between visceral and parietal pleural space.
- Most common causes: CHF, infection, malignancy, renal, or hepatic failure.
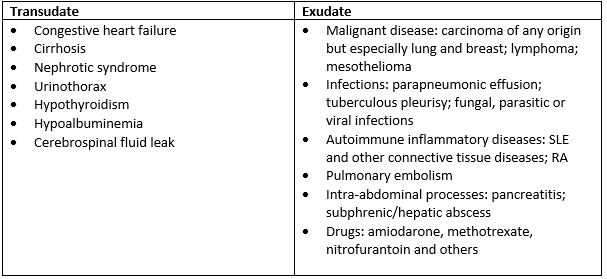
- Transudative (systemic factors) management focuses on the mechanism causing fluid accumulation.
- Exudative (pleural surfaces or adjacent lung) management based on cause – see below.
Diagnostic Process
- Etiology of Pleural Effusions:
- Symptoms: dyspnea, chest pain, cough.
- Physical findings, can include diminished breath sounds, asymmetrical chest expansion, decreased vocal fremitus, and dullness to percussion.
- Chest X-ray (CXR) needs 200mL of fluid in the pleural space on an AP CXR and 75mL on a lateral to detect.
- If the entire hemithorax looks like a “white-out” on CXR, look for mediastinal shift, as the patient may need a prompt thoracentesis for relief of symptoms (tension hydrothorax.)
- Ultrasound useful.
- CT chest, to further evaluate the source of the patient’s symptoms.
- A diagnostic thoracentesis can be performed in patients with new pleural effusions or in patients with known but worsening pleural effusions.
- Pleural fluid analysis using Light’s criteria suggest exudative if:
- Pleural Total Protein/Serum Total Protein ratio > 0.5
- Pleural LDH/Serum LDH ratio > 0.6
- Pleural LDH level > 2/3 upper limit of the laboratory’s reference range of serum LDH
Recommended Treatment
- Treatment of the underlying cause (i.e., diuresis for heart failure.)
- Indications for thoracentesis in the ED (or by interventional radiology where available.)
- Unstable patient, respiratory distress.
- New effusions >10mm.
- Complicated parapneumonic effusions.
- Patients with empyema.
- Do not drain more than 1 liter of fluid at a time as can lead to re-expansion pulmonary edema. Use ultrasound guidance to decrease complications.
- Indications for thoracostomy chest tube drainage in pleural infection:
- Frank pus/turbid pleural fluid on sampling.
- Presence of organisms identified by Gram stain and/or culture from pleural fluid sample.
- Pleural fluid pH <7.2.
Criteria For Hospital Admission
- Patients with new pleural effusion or pleural effusion causing hemodynamic instability or respiratory distress.
Criteria For Transfer To Another Facility
- Transfer to facility with respirology or thoracic/general surgery service if required.
Criteria For Close Observation And/or Consult
- Undiagnosed effusion after initial assessment and thoracentesis.
- Parapneumonic effusion, particularly if complicated.
- Proven or suspected malignant effusion and symptom palliation.
- Recurrent effusions of any etiology.
- Effusion in the outpatient primary care setting where basic investigations may not be accessible.
- Respirology or thoracic surgery should be involved in care of all patients requiring chest tube drainage.
Criteria For Safe Discharge Home
- Patients with a known pleural effusion presenting with complaints unrelated to the effusion may be discharged home, ensuring they have appropriate follow up.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
High quality evidence for ultrasound guidance for thoracentesis, moderate quality for indications for thoracentesis and chest tube insertion as management for pleural effusions.
Low quality evidence for approach to diagnosis (including use of Light’s criteria), based on observational studies and clinical practice.
Related Information
OTHER RELEVANT INFORMATION
Malignant Pleural Effusion Patient Education Sheet from ATS: https://www.thoracic.org/patients/patient-resources/resources/malignant-pleural-effusions.pdf
Reference List
Beaudoin S, Gonzalez AV. Evaluation of the patient with pleural effusion. Canadian Medical Association Journal. 2018;190(10).
Davies HE, Davies RJ, Davies CW. Management of pleural infection in adults: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010;65(Suppl 2):ii41–ii53.
Diaz-Guzman E, Dweik RA. Diagnosis and management of pleural effusions: A practical approach. Comprehensive Therapy. 2007;33(4):237–46.
John HE. Diagnostic evaluation of a pleural effusion in adults: Initial testing [Internet]. UpToDate. [cited 2022Nov29]. Available from: https://www.uptodate.com/contents/diagnostic-evaluation-of-a-pleural-effusion-in-adults-initial-testing?search=pleural+effusion&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
Soni NJ, Franco R, Velez MI. Ultrasound in the diagnosis and management of pleural effusions. Journal of Hospital Medicine. 2015;10(12):811–6.
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Oct 10, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.