Pleurisy (Diagnosis + Treatment)
Respiratory
Context
- Pleurisy is inflammation of parietal pleura and commonly presents as pleuritic chest pain.
- Pulmonary Embolism is the most common life-threatening cause of pleuritic pain. Approximately 5-21% of patients that have pleuritic pain will have a pulmonary embolism. Myocardial infarction, pneumothorax, pneumonia and pericarditis should also be on the differential when a patient presents with pleuritic chest pain.
- It is essential to rule out life-threatening causes of pleuritic pain; pleurisy is a diagnosis of exclusion.
- The most common cause of pleurisy are viruses (including influenza, RSV, CMV, Epstein-Barr, adenovirus among others).
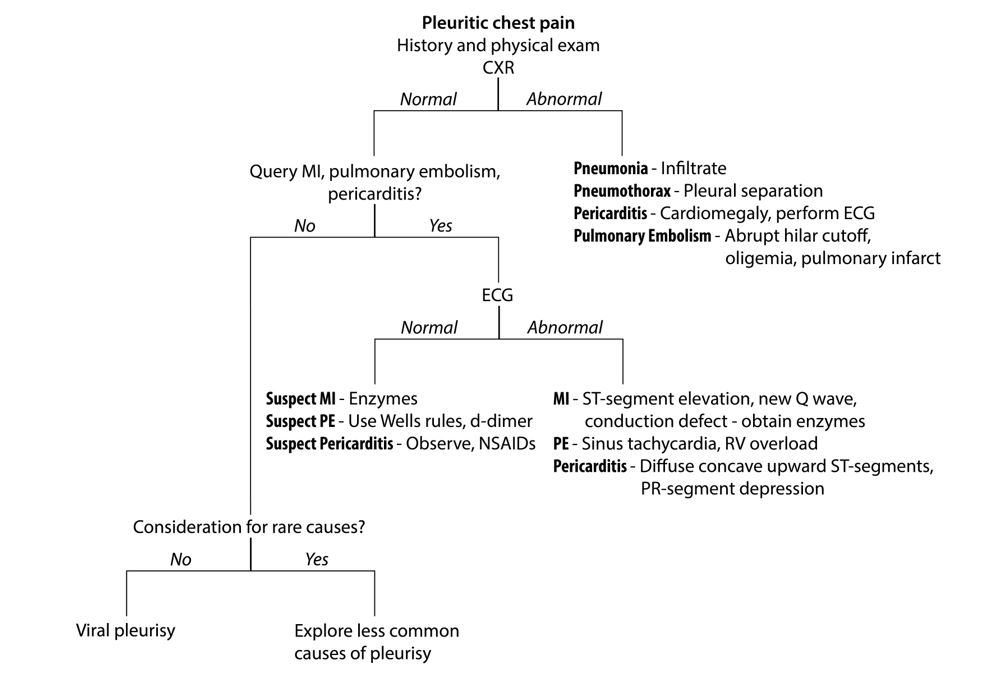
“Algorithm for the outpatient diagnosis of pleuritic pain.” From Kass, S., Williams, P. and Reamy, B., 2007. Pleurisy. American Family Physician, 75(9), pp.1357-1362.
Diagnostic Process
- Once life-threatening diagnoses are ruled out, the differential for pleurisy is broad and includes malignancy, asbestosis, rheumatoid pleuritis, lupus pleuritis, post-cardiac injury syndrome, infectious etiologies and chronic renal failure.
Key aspects to elucidate on history include:
- Arthralgias, arthritis, prior connective tissue diagnoses (connective tissue disease-induced pleuritis).
- Medication history (drug-induced pleuritis).
- Repeated episodes of fever associated with abdominal, chest or joint pain, family history of Mediterranean fever (familial mediterranean fever).
- Recent heart attack, cardiac procedure or trauma (post-cardiac injury syndrome).
- Fever, malaise, night sweats (tuberculous pleurisy), viral symptoms (viral pleurisy).
- History of malignancy (metastasis to the pleura).
Physical Exam
- A pleural friction rub may be auscultated, or there may decreased breath sounds in the presence of a pleural effusion.
Investigations
- CBC, electrolytes, troponin, CXR, ECG will typically be required at the minimum. A myocardial infarction can less commonly present with pleuritic chest pain, so it should be on the differential. Effusions are normally seen connective tissue disorders, tuberculous pleuritis and are sometimes seen in drug-induced pleuritis.
- If CXR shows pleural effusion, the pleural fluid should be analyzed for pH, glucose, cell count, lactate dehydrogenase, and bacterial Gram stain and cultures.
- The appearance of blood can suggest cancer, pulmonary embolus, trauma or hemothorax depending on the hematocrit levels.
- Light’s criteria can also be used to established if the fluid is exudate or transudate, which further guides the differential for pleural effusion.
Recommended Treatment
- To manage the pain associated with pleurisy, NSAIDs are the mainstay. Indomethacin 50 – 100 mg PO TID is the agent of choice. Otherwise, management depends on the cause.
- Pleural Effusion: Diagnostic and therapeutic thoracentesis should be done.
- Viral: Pain management and supportive care.
- Below are rarer causes of causes of pleurisy that would likely need to be managed in collaboration with a specialist.
- Drug-induced pleuritis: Drug agent should be stopped. Procainamide and hydralazine are the drugs most commonly associated with drug-induced lupus pleuritis.
- Asbestosis: Smoking cessation is recommended.
- Familial Mediterranean fever: Colchicine 1.2 – 2 mg PO qd or 0.6 – 1 mg PO BID.
- Post-cardiac injury syndrome: NSAIDs: Ibuprofen 600 – 800 mg PO q 6- 8 hrs with gradual tapering of the total daily dose by 400 – 800 mg each week for 3-4 weeks.
- Lupus pleuritis: corticosteroids are sometimes used, although the optimal dosing has not yet been established. Corticosteroids have not been proven to be beneficial in the treatment of rheumatoid pleuritis.
- Tuberculous pleuritis: long-term antibiotics required (selection dependent on local resistance patterns).
Related Information
OTHER RELEVANT INFORMATION
https://www.amboss.com/us/knowledge/Pleural_effusion/
https://www.aafp.org/afp/2007/0501/p1357.html
https://www.merckmanuals.com/home/lung-and-airway-disorders/pleural-and-mediastinal-disorders/pleural-effusion
Reference List
Dellaripa, P. and Danoff, S., n.d. Pulmonary manifestations of systemic lupus erythematosus in adults. [online] UpToDate. Available at: <https://www.uptodate.com/contents/pulmonary-manifestations-of-systemic-lupus-erythematosus-in-adults/print> [Accessed 4 January 2022].
He, Y. and Sawalha, A., 2018. Drug-induced lupus erythematosus: an update on drugs and mechanisms. Current Opinion in Rheumatology, 30(5), pp.490-497.
Huggins, J. and Sahn, S., 2004. Drug-induced pleural disease. Clinics in Chest Medicine, 25(1), pp.141-153.
Jeon, D., 2014. Tuberculous Pleurisy: An Update. Tuberculosis and Respiratory Diseases, 76(4), p.153.
Kass, S., Williams, P. and Reamy, B., 2007. Pleurisy. American Family Physician, 75(9), pp.1357-1362.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Moderate quality evidence for use of NSAIDs to manage pain in the context of pleurisy. It was graded as a B (inconsistent or limited quality patient-oriented evidence) based on the SORT scale, a scale used by the AAFP journal.
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jan 09, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.