Proximal and Midshaft Humeral Fractures in Adults
Orthopedic, Trauma
First 5 Minutes
- Assess neurovascular status.
- Assess for evidence of open fracture.
- Assess joint above and joint below.
Context
Humeral fractures can occur proximally, in the shaft (diaphysis), or distally.
Humeral Shaft Fractures:
Mechanism of Injury:
- Commonly a direct blow to the arm, severe twist, or FOOSH.
- Typical fracture patterns include transverse, oblique, or spiral fractures.
Risk Factors:
- High energy trauma.
- Pathologic fracture (benign tumors, unicameral cysts, malignancy).
Clinical features:
- Severe focal pain/tenderness.
- Swelling.
- Immobility.
- Shortening or rotation.
- Bony tenderness and swelling without obvious deformity (incomplete fracture).
Complications:
- Acute: radial nerve injury (wrist drop).
- Neurapraxia (most common); self-resolving in 80-90% over 6 to 9 months.1
- Neer Classification2 – based on the anatomical relationship of the four major segments of the proximal humerus: anatomical neck, surgical neck, greater tuberosity, and lesser tuberosity.
- Fractures are classified according to number of segments displaced (displacement occurs when a segment is angulated more than 45 degrees or displaced > 1cm from normal anatomical position).
- One-part fractures – no fragments are displaced.
- Two-part fractures – one displaced fragment.
- Three-part fractures – two displaced fragments but humeral head remains in contact with glenoid.
- Four-part fractures – three or more displaced fragments and dislocation of articular surface from the glenoid.
- Fractures are classified according to number of segments displaced (displacement occurs when a segment is angulated more than 45 degrees or displaced > 1cm from normal anatomical position).
Proximal Humeral Fractures:
Mechanism:
- FOOSH.
- Direct blow to the lateral side of the arm.
- Axial load transmitted through the elbow.
- High-energy mechanisms and polytrauma (younger patients).
Clinical Features:
- Shoulder adduction, internal rotation and elbow flexion.
- Guarding.
- Tenderness, hematoma, ecchymosis, deformity, or crepitus over fracture site.
Complications:
- Acute: axial nerve, brachial plexus, or axillary artery injury.
- Chronic: adhesive capsulitis, avascular necrosis, heterotrophic bone formation (myositis ossificans, especially following multiple attempts to reduce fracture-dislocations).
Differential Diagnosis:
- Shoulder fracture-dislocation
- Glenohumeral dislocation
- AC joint separation
- Rotator cuff tendon tear
- Soft tissue injury – muscle strain, ecchymosis
Diagnostic Process
- Complete neurovascular exam.
- Assess for evidence of open fracture.
- Imaging:
- Proximal humerus fractures in adults:
- Plain radiographs of the shoulder3:
- True AP view
- Axillary view
- Scapular-Y view
- Plain radiographs of the shoulder3:
- CT scan is recommended for:
- fracture dislocations
- humeral head-splitting fractures
- comminuted fractures
- Midshaft fractures in adults:
- Lateral and AP radiographs are necessary to evaluate the amount of angulation/displacement of the fracture.
- Include radiographs of shoulder and elbow if injury to these joints cannot be ruled out by physical exam.
- Proximal humerus fractures in adults:
Recommended Treatment
Non-pharmacological, including surgical treatments
- Appropriate evaluation for additional traumatic injuries.
- Appropriate analgesia.
- Support of injured extremity to ensure patient comfort.
Most proximal and midshaft humeral fractures are non-displaced, can be treated conservatively, and do not require surgical management3.
Proximal humeral fractures:
- Immobilization in a standard sling or collar and cuff sling.
- Ice to reduce pain and swelling.
- Patients may prefer to sleep semi-recumbent (e.g., in a reclining chair or propped up with pillows/wedge in bed) with a sling.
- Repeat clinical evaluation and radiographs in 1 week.
- Closed reduction of fracture fragments is not recommended due to the forces exerted by insertion muscles on the humerus.
Most humeral shaft fractures can be treated initially in a coaptation splint4,5. Some spiral, oblique and comminuted fractures require traction, in addition to splinting, to achieve appropriate alignment.
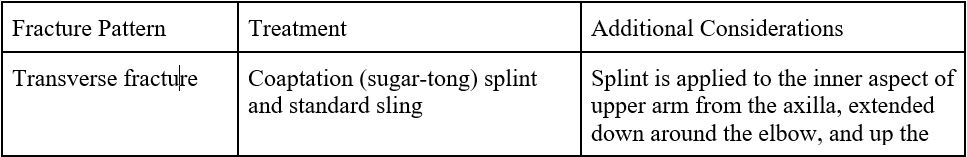
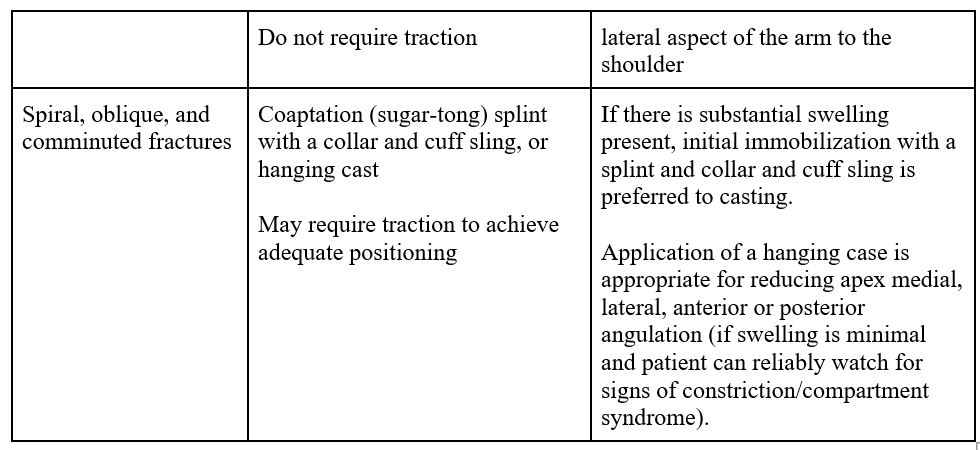
Midshaft humeral fractures:
- Midshaft humerus fractures associated with vascular injury or open fractures require immediate surgical referral. Other absolute indications for referral include:
- Fractures associated with articular injury.
- Brachial plexus injuries.
- Associated ipsilateral forearm fractures (e.g., floating elbow).
- Pathological fractures.
- Concomitant major traumatic injuries.
- High-velocity gunshot injuries.
- Fracture associated with severe soft tissue injuries or significant skin involvement.
- Holstein Lewis Fractures (displaced spiral shaft fractures) generally require surgical evaluation due to their high association with radial nerve injury.
Criteria For Hospital Admission
Consider hospital admission for patients with:
- Multiple traumatic injuries that require inpatient treatment/observation.
- Open fractures.
- Vascular or neurologic compromise.
- Fractures in the elderly that culminate in loss of independence and ability to cope.6
Criteria For Transfer To Another Facility
- Consider transport to another facility if the patient has a severe humeral fracture that requires specialized care that is unavailable at the current facility.
- Provide appropriate analgesia during transport.
Criteria For Close Observation And/or Consult
- Referral to orthopedic surgeon recommended for patients with Neer 2-4 part proximal humeral fractures, or those with anatomical neck fractures.
- Emergent orthopedic consultation is indicated for all open fractures, fracture dislocations, severely displaced or comminuted fractures, fractures associated with ipsilateral forearm fractures, and neurovascular injuries.
Criteria For Safe Discharge Home
- Most humeral injuries can be discharged home with appropriate orthopedic specialty follow-up.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Recommendations based on results of peer reviewed studies in orthopedic literature.
Related Information
Reference List
Walls, R, editor-in-chief. Rosen’s emergency medicine: concepts and clinical practice. Tenth edition. Philadelphia: Elsevier; 2023.
Neer CS. Classification and evaluation. JBJS. 1970;52:1077-89.
Vachtsevanos L, Hayden L, Desai AS, Dramis A. Management of proximal humerus fractures in adults. World journal of Orthopedics. 2014 Nov 11;5(5):685.
Sarmiento A. Functional bracing of fractures of the shaft of the humerus. Orthopedic Trauma Directions. 2008 Jan;6(01):33-7.
Rutgers M, Ring D. Treatment of diaphyseal fractures of the humerus using a functional brace. Journal of orthopaedic trauma. 2006 Oct 1;20(9):597-601.
Roux A, Decroocq L, El Batti S, Bonnevialle N, Moineau G, Trojani C, Boileau P, De Peretti F. Epidemiology of proximal humerus fractures managed in a trauma center. Orthopaedics & Traumatology: Surgery & Research. 2012 Oct 1;98(6):715-9.
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Mar 13, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.