Schizophrenia
Psychiatric and Behaviour
First 5 Minutes
Suicide and suicide attempts are higher in schizophrenic patients.
Consider compliance issues and substance use for exacerbations.
Neuroleptic malignant syndrome (NMS) is a medical emergency which can occur after administering antipsychotic medications:
- Altered mental status,
- Muscle rigidity,
- Hyperthermia, and
- Autonomic instability = hypertension or hypotension/tachycardia.
- Can cause rhabdomyolysis.
- Management includes stopping the culprit medication and supportive care (e.g., hydration, treat symptoms, monitor vitals and organ functioning) if this occurs.
Context
- Schizophrenia is a disabling, chronic mental disorder that can present as psychosis, flattened affect, anhedonia, and disorganized thoughts/behaviours.
- The onset of schizophrenic symptoms late adolescence or early adulthood and can be abrupt or gradual.
- The main reasons for presentation:
- Psychotic symptoms.
- Agitation.
- Related mental disorder: substance use disorder, anxiety, depression.
- Physical disorder: acute injury, infection.
Diagnostic Process
Schizophrenia is diagnosed clinically.
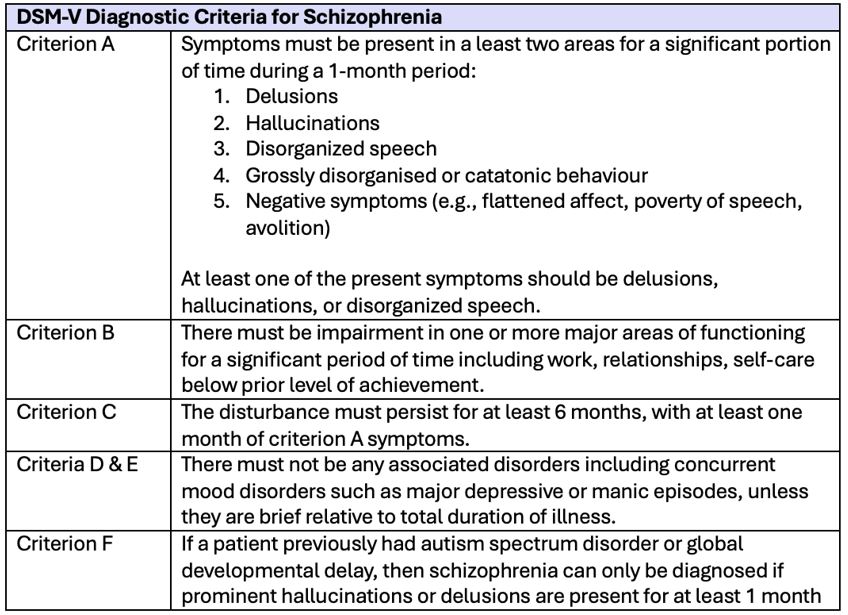
Table 1: DSM-V Criteria for Diagnosing Schizophrenia.
Associated signs and symptoms include cognitive deficits, reduced attention, irritable mood, impaired motor coordination, and left-right confusion.
Differential diagnoses to consider when a patient presents with the above symptoms include:
- Substance or medication-induced psychosis.
- Psychosis secondary to a medical condition (e.g., epilepsy, lupus, dementia, endocrine disorders, autoimmune disorders, neoplastic disorders).
Investigations to consider if initial presentation or acute change in behaviour:
- Complete blood count.
- Metabolic panel.
- Extended electrolytes.
- Drug and alcohol screening.
- TSH.
- C-Reactive Protein or ESR.
- Syphilis testing.
- CT head.
- +/- Lumbar puncture.
- +/- Electroencephalography (EEG).
Recommended Treatment
Patients should receive a psychiatric evaluation rapidly which includes a risk assessment for suicide.
Acute agitation is treated as described in Clinical summaries:
- Management of agitated patient in the Emergency Department – Adult
- Treating Acute Agitation with Ketamine in the Emergency Department
- Management of Agitation or Aggression – Pediatric
Initiating antipsychotics:
Generally left for psychiatrists or family doctors. Some tips to consider when treating schizophrenia patients with antipsychotics:
- Lower dose recommended due to better treatment response and lower risk of adverse effects.
- Consider past treatments and patient preference.
- No consensus on which antipsychotic to administer or a precise dose.
- Adverse effects of medication include sedation, acute dystonia, akathisia (inability to stand still), parkinsonism (e.g., tremor, slow movement, rigidity, postural instability).
Consider for admission to psychiatry but if symptoms are mild and they are able to care for themselves with good family support and close follow-up, they may receive a comprehensive plan which includes follow-up with a Psychiatrist, social support services, therapy (e.g., cognitive behavioural therapy), assertive community treatment, and family support upon discharge.
Compliance with treatment is a protective factor for suicide risk; however, non-adherence is unfortunately common in schizophrenia patients.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Schizophrenia in an emergency medicine context.
Antipsychotic drug of choice and dose.
Diagnosis and risk factors.
Related Information
OTHER RELEVANT INFORMATION
https://emergencycarebc.ca/clinical_resource/acute-psychosis-diagnosis/
https://emergencycarebc.ca/clinical_resource/neuroleptic-malignant-syndrome-diagnosis-treatment/
https://emergencycarebc.ca/clinical_resource/suicide-risk-assessment/
https://emergencycarebc.ca/clinical_resource/management-of-agitation-or-aggression-pediatric/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4786236/
https://www.sciencedirect.com/science/article/pii/S0163834399000031#aep-section-id24
https://www.tandfonline.com/doi/abs/10.1080/17522439.2021.1912815
Reference List
Stilo SA, Murray RM. Non-genetic factors in schizophrenia. Current Psychiatry Reports. 2019;21(10). doi:10.1007/s11920-019-1091-3
Remington G, Addington D, Honer W, Ismail Z, Raedler T, Teehan M. Guidelines for the pharmacotherapy of schizophrenia in adults. The Canadian Journal of Psychiatry. 2017;62(9):604–16. doi:10.1177/0706743717720448
Lawrence RE, Bernstein A. Schizophrenia and emergency medicine. Emergency Medicine Clinics of North America. 2024 Feb;42(1):93–104. doi:10.1016/j.emc.2023.06.012
Correll CU, Martin A, Patel C, Benson C, Goulding R, Kern-Sliwa J, et al. Systematic literature review of schizophrenia clinical practice guidelines on acute and maintenance management with antipsychotics. Schizophrenia. 2022;8(1). doi:10.1038/s41537-021-00192-x
Tandon R, Gaebel W, Barch DM, Bustillo J, Gur RE, Heckers S, et al. Definition and description of schizophrenia in the DSM-5. Schizophrenia Research. 2013 Oct;150(1):3–10. doi:10.1016/j.schres.2013.05.028
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jun 04, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.