Seizure in Adults
Neurological
First 5 Minutes
- ABCD
- Airway – suction, lateral decubitus positioning.
- Breathing – supplemental oxygen as patient may become apneic.
- Circulation.
- Dextrose – Bedside glucose reading.
- Monitors – get to monitored bed/monitors attached.
- Oxygen – Supplemental O2.
- Vital signs.
- IV access.
- Consider ECG g.
- Treatment of status epilepticus (see “Recommended Treatment” below”).
Context
- Seizures are sudden changes in neurologic function caused by inappropriate discharge of electrical activity in the brain.
- Epilepsy is a clinical syndrome where an individual experiences two or more provoked seizures more than 24 hours apart.
- Status epilepticus is characterized by seizures lasting more than 5 minutes or recurrent seizures, without return to baseline mental status.
- Lifetime seizure risk is 2-5%, and seizures account for 1-2% of ED visits.(1)
Primary goals of the ED physician managing seizure in the adult:
- Look for and treat reversible causes.
- Identify and rapidly manage status epilepticus.
Diagnostic Process
Known Seizure history
- Blood glucose, pertinent anticonvulsant drug levels.(2)
- History is important to determine cause:
- Often caused by lack missed medication doses.(2)
- Obtain serum drug level and consider loading dose.
- If serum drug level not available (e.g. Leviteracetam, lacosamide) – give usual dose.
- Consider ruling-out secondary causes (see workup for new seizure).
- Look for change in previous seizure pattern (in this case approach as new seizure).
- Often caused by lack missed medication doses.(2)
New Seizure
- Rule-out seizure mimics (syncope, CVA, migraine, psychogenic nonepileptic seizures).
- Determine if provoked vs unprovoked (See Table 1).
Imaging(2)
- CT Head (NCCT) for all adult patients with:
-
- First ever seizure.
- Change in established seizure pattern.
- Concern for acute intracranial process (persisting focal deficits, head trauma, anticoagulant use, history of cancer).
Other Investigations:
- EEG: not routinely available. Consider for persistent/refractory status epilepticus, evaluation of non-convulsant status epilepticus.
- Site-specific injury for suspect injuries (i.e., spinal trauma, shoulder dislocations, etc.).
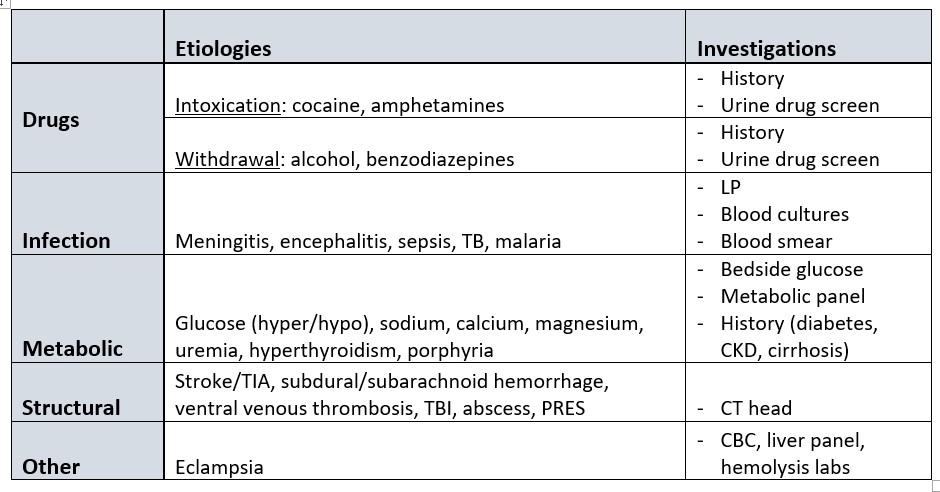
Table 1 – Etiology and Investigations for Provoked Seizure
Recommended Treatment
Status Epilepticus (SE)
Step 1: Abortive therapy
- Preferred agents based on access.(3)
- Lorazepam (IV)
- Midazolam (IM)
- Diazepam (IV / rectal)
- Lorazepam may carry lower risk than diazepam for continuation of status epilepticus requiring different drug or general anesthesia.(4)
- Lorazepam is better than phenytoin for cessation of seizures.(4)
Step 2: Anti-epileptic drug (AED)
All patients in SE require AED in addition to benzodiazepine abortive therapy, whether or not the seizure has aborted.(3) Required to prevent recurrence, or for failure of emergent initial therapy.
- Adult, no seizure history
- Phenytoin/fosphenytoin.(3)
- Adult, epilepsy
- Valproate sodium.(3)
- IV bolus of patient’s maintenance medication, if available may be used first.
- Other agents: phenobarbital, levetiracetam, continuous infusion midazolam.
If seizure cessation after step 2, stop.
If seizure activity persists, patient has refractory SE. Continue to step 3.
Step 3: Refractory Status Epilepticus (20-60 min after initiation of second agent)(3)
- Option 1: Repeat bolus of AED chosen in step 2.
- If trial of option 1 fails, proceed to option 2.
- Option 2: Continuous infusion AED
- Medication options: Midazolam, propofol, phenobarbital.
- Note: Continuous infusion AEDs generally requires ventilatory assistance and cardiovascular monitoring. Vasopressor agents may be required for hemodynamic support.
- If trial of option 2 fails, trial with a second continuous infusion agent.
- Patients in this category should be admitted to ICU/neuro ICU, or transferred to a facility with this service.
Aborted Seizure (Non-status epilepticus)
Patient with documented seizure history/disorder:
- Home anti-epileptic drugs (AED) – May require adjustment in maintenance dose.
- Requires follow-up with Neurologist/PCP.
First-time seizure:
- Not all with first-time seizures require preventative AED. Those with high-risk features may receive treatment(5), though some experts believe that prophylactic AEDs should not be routinely started in the ED.(6)
- High-risk features include(5):
- Epileptiform activity on EEG.
- Abnormal brain imaging.
- Nocturnal seizure.
- Severe head trauma.
- Epilepsy syndrome (the signs and symptoms classic for an epileptic condition).
- 2 unprovoked seizures >24 hours apart.
- If high-risk criteria are met, and AEDs are started in the ED, initiating treatment with monotherapy agent is advised, as per Table 1 in AAFP article (medication will vary by seizure type). https://www.aafp.org/pubs/afp/issues/2017/0715/p87.html
- Consultation with a specialist is recommended for first-time unexplained seizure and those with high risk seizures.
Criteria For Hospital Admission
- Pregnant > 20 weeks.
- New focal abnormality.
- Mental status not returning to baseline.
- Refractory SE.
Criteria For Transfer To Another Facility
- If a patient requires admission and neurology is not available in house, transfer once stabilized in consultation with neurology.
- Refractory SE, patient should be monitored in ICU/neuro ICU, which may require transfer once stabilized.
Criteria For Close Observation And/or Consult
- Consult neurology (or arrange for rapid follow-up) if:
- New seizure of undetermined etiology.
- History of seizure with new change in seizure pattern.
- Consult ICU/neuro-ICU if:
- Refractory SE.
Criteria For Safe Discharge Home
- Must make full neurological recovery.
- All patients with first episode of generalized seizure should be counselled to stop driving and this conversation should be documented.(6)
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
There is a Cochrane review for initial pharmacotherapy of status epilepticus, however guidelines are based on expert consensus.
Related Information
OTHER RELEVANT INFORMATION
Patient information:
- After a first, unprovoked seizure(5):
- Risk of recurrence: 50% over 5 years. 1/3 of this risk is within first year.
- Adult > 65: Risk of recurrence: 80% lifetime, 53% within first year.
- Initiating AED therapy decreases risk of recurrence by 35% over next 2 years.
- Certain activities are high-risk and should be avoided prior to consultation with neurologist. These should be discussed prior to discharge and include:
- Driving
- https://www2.gov.bc.ca/gov/content/transportation/driving-and-cycling/roadsafetybc/medical-fitness/medical-prof/med-standards/17-seizures#17.6.1
- Return to driving laws vary by seizure type, and class of driver (commercial vs non-commercial).
- Operating heavy machinery.
- Swimming.
- Anything activity where a seizure would put themselves or others at-risk.
- https://www2.gov.bc.ca/gov/content/transportation/driving-and-cycling/roadsafetybc/medical-fitness/medical-prof/med-standards/17-seizures#17.6.1
- Driving
A number of handouts are available from the BC Epilepsy Society including a variety of information sheets, seizure first aid and safety and wellness guides: https://bcepilepsy.com/information-sheets-brochures/
- After a first, unprovoked seizure(5):
Related Information
Reference List
Clinical Policy: Critical Issues in the Evaluation and Management of Adult Patients Presenting to the Emergency Department with Seizures. Ann Emerg Med. 2004;43(5):605–25.
Tintinalli, J.E., Stapczynski, J.S., Ma, O.J., Yealy, D.M., Meckler, G.D., Cline DM. Tintinalli’s Emergency Medicine 8th Ed. 8th ed. McGraw-Hill; 2016.
Brophy GM, Bell R, Claassen J, Alldredge B, Bleck TP, Glauser T, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012 Aug;17(1):3–23.
Prasad M, Krishnan PR, Sequeira R, Al-Roomi K. Anticonvulsant therapy for status epilepticus. Cochrane database Syst Rev. 2014 Sep 10;2014(9).
Liu G, Slater N, Perkins A. Epilepsy: Treatment Options. Am Fam Physician. 2017 Jul 15;96(2):87–96.
Breen DP, Dunn MJG, Davenport RJ, Gray AJ. Epidemiology, clinical characteristics, and management of adults referred to a teaching hospital first seizure clinic. Postgrad Med J. 2005 Nov;81(961):715–8.
Smith EF, Cantrill S V., Campbell M, Colucciello SA, Dalsey WC, Fesmire FM, et al. Clinical policy for the initial approach to patients presenting with a chief complaint of seizure who are not in status epilepticus. American College of Emergency Physicians. Ann Emerg Med. 1997;29(5):706–24.
Kwon CS, Wong B, Agarwal P, Lin JY, Mazumdar M, Dhamoon M, et al. Nonelective hospital admissions, discharge disposition, and health services utilization in epilepsy patients: A population-based study. Epilepsia. 2020 Sep 1;61(9):1969–78.
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Feb 02, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.