Suicide Risk Assessment
Psychiatric and Behaviour
Context
- Suicide assessment in the ED is imprecise. 40% of patients who attempted or completed suicide had visited ED in the prior 12 months and up to 10% of patients with medical complaints endorse suicide ideation only when asked (US study).
- No rule is useful in isolation and no clinical summary can replace physician judgment but they may help physicians reach better decisions. Mental health resources are institutionally and geographically specific. Each center has to determine its own criteria for safety of discharge versus transfer to a higher level of intervention using the general principles described.
Steps for patient presenting to ED with suicide risks
1. ASSESS for presence of acute medical conditions/impaired mentation/medical incompetence
1. Medical Rx for delirium, violence, altered mental status…
a. Vital signs, Toxidromes, Bloodwork/ECG/drug screen as indicated
b. Chemically restrain [and physically] if necessary for diagnosis/treatment
2. Involuntary Hold until medically cleared if (1) is present
3. Obtain collateral input/healthcare representative if medically incompetent/mentally impaired
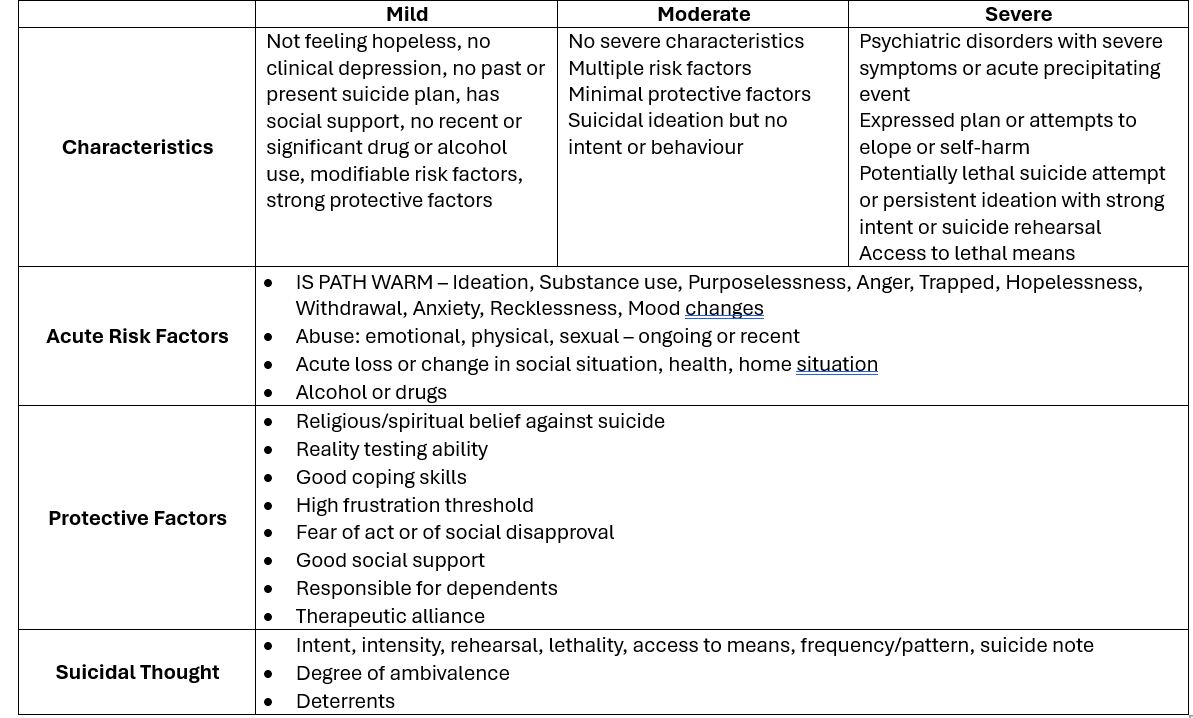
2. BALANCE suicide risk factors [Chart 1 below]:
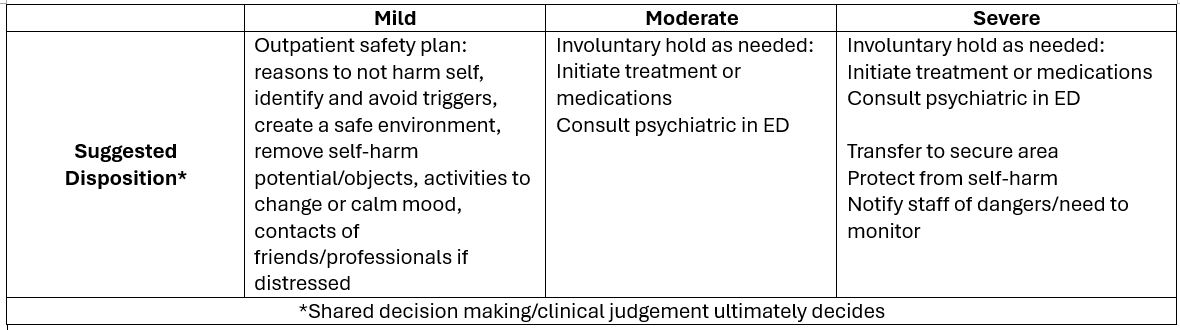
1. MILD: suitable to discharge after safety plan formulated/agreed by patient
2. MODERATE: requires psychiatry consult with involuntary hold as necessary
3. SEVERE: requires close monitoring for safety/elopement risks until psychiatry assessment
3. COMMUNICATE with staff, psychiatry if consulted, patient and his/her support of decision
4. DOCUMENT
1. Risk level rationale, treatment initiated, disposition plans
2. All involuntary hold and treatment forms if utilized
3. Communication with Psychiatry re: consult and expected time for psychiatry assessment
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Most studies are US based with different demographics and are subjective/qualitative in nature.
Additional Suggestions
- Apps or walls charts of risk factors serve as useful reminders
- Beware of bias due to location of patient or past history of frequent visits/manipulative behavior
- Chronic [e.g. drug use, socio-demographics] risk factors though less important should be documented
- Defensive and de-escalation skills training should be available/encouraged for staff
Risk Assessment Chart
Related Information
OTHER RELEVANT INFORMATION
Betz ME, Boudreaux ED. Managing Suicidal Patients in the Emergency Department.
Reshetukha, et al. Improving suicide risk assessment in the emergency department through physician education and a suicide risk assessment prompt.
CAMH Suicide Prevention and Assessment Handbook
Suicide Prevention Resource Center (US)
SuicideAssessment Five-step Evaluation and Triage – Substance Abuse and Mental Health Services Administration (US)
Relevant Resources
RELEVANT RESEARCH IN BC
Procedural Sedation and Analgesia System Response to Toxicologic EmergenciesRESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Aug 27, 2018
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.