Unstable Angina/Non-ST Elevation Myocardial Infarction (UA-NSTEMI) Diagnosis
Cardinal Presentations / Presenting Problems, Cardiovascular, Critical Care / Resuscitation
Context
Definition1:
- Acute Coronary Syndrome includes:
- ST Elevation Myocardial Infarction (STEMI).
- Non-ST Elevation Myocardial Infarction (NSTEMI).
- Unstable Angina (UA).
- Each includes clinical symptoms and signs of unstable ischemia.
- +/- new ECG ischemic changes.
- Differentiator is elevated troponin in STEMI / NSTEMI.
- No change in troponin in UA.
- Clinical Classification of MI:
- Type 1: Atherosclerotic plaque rupture.
- Type 2: demand ischemia: O2 supply-demand mismatch.
- Type 3: ECG ischemic features but unexpected death prior to drawing troponins.
- Type 4a/4b: MI related to percutaneous coronary intervention.
- Type 5: MI related to CABG.
- Elderly, diabetics, and women can have atypical presentations and warrant careful evaluation.
Diagnostic Process
- Patient outcomes improved with early diagnosis and treatment2.
- Management often concurrent with diagnostic process.
- Rapid assessment and initial management = < 10 mins of presentation (includes history, physical, ECG, troponin bloodwork drawn).
- Determine if ACS and if ACS: UA versus NSTEMI versus STEMI.
- Features suggestive of ACS angina:
- Rest angina (‘usually’ greater than 20 mins), new onset angina with marked impairment in physical activity, progressively worsening baseline angina.
- NSTEMI and UA diagnosis is made with or without ECG changes. Difference between them is degree of ischemia able to cause myocardial damage and releasing troponin.
- UA: Clinical presentation of ischemic symptoms but no elevation of troponins +/- new ischemic ECG changes. Clinical history very important.
- NSTEMI: Clinical presentation of ischemic symptoms with elevation of troponins +/- new ischemic ECG changes.
- History:
- Ischemic Chest Pain Characteristics:
- Gradual onset, worse with exertion, no changes with respiration or position, may have some relief with nitroglycerin.
- Pain can be difficult to describe – “squeezing, tightness, pressure, constriction, crushing, burning, lump in throat”. Usually not described as sharp.
- Radiation of pain to other parts of body – upper arms, neck, back.
- Diffuse pain rather than specific spot
- Stable angina usually 2-5 mins and relieved with rest or Nitroglycerin.
- UA = new onset, worsening pain (intensity/duration) with less exertion/at rest; less relief with NTG/rest.
- ACS chest pain generally lasts longer than 30 mins.
- Ischemic Chest Pain Characteristics:
*Note: Relief of chest pain following trial of GI cocktail of antacid (+/- viscous lidocaine) or relieve with nitroglycerin cannot reliably rule in/out ischemic chest pain.
- Non-ischemic chest pain (less likely ACS):
- Pleuritic pain related to respiration.
- Localizable with finger.
- Reproducible.
- Constant lasting days.
- Pain lasting few seconds.
- Associated symptoms: shortness of breath, nausea, indigestion, vomiting, diaphoresis, dizziness, fatigue.
- Past medical history: prior ACS, vascular disease.
- Risk factors: age, male, diabetes, hypertension, dyslipidemia, smoking, cocaine use, family history positive ACS or sudden death.
Elderly, diabetics and women may not have chest pain but instead dyspnea, nausea or vomiting, weakness, etc.
- Physical Exam:
- Targeted:
- Cardiogenic shock: hypotension, tachycardia, altered level of consciousness, cool/pale skin.
- Heart Failure: elevated JVP, lung crackles, hypotension, tachycardia, mitral regurgitation murmur.
- Neuro examination: helps in decision making regarding possible use of thrombolytic therapy.
- Otherwise full cardiac, respiratory, abdominal examination is warranted.
- Targeted:
- Differential Diagnosis:
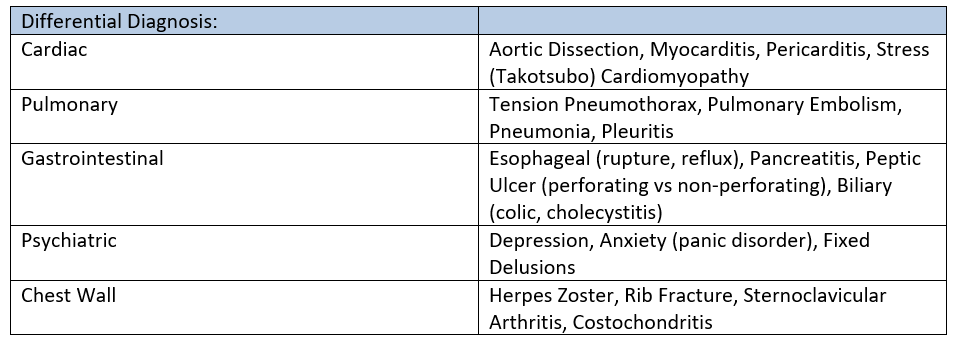
Table 1: Adapted from UpToDate: Initial evaluation and management of suspected acute coronary syndrome (myocardial infarction, unstable angina) in the emergency department.
- Investigations specifically for ACS1:
- Troponin:
- Abnormal when >= 99 percentile upper limit normal (varies per assay)
- Use in clinical context, non-specific elevations seen (e.g. in Chronic Kidney Disease, Sepsis).
- In patients with chronic elevations, use rise or fall in troponin values.
- Serial testing is important. Most patients with acute MI can be ruled out by 6 h. If high degree suspicion 12 h sample should be taken.
- Recommended:
- Measure at first presentation.
- Repeat in 3-6 h (80% patients found to have elevation in 2-3 h).
- Shorter periods for high sensitivity troponins.
- Troponin:
Don’t delay treatment in suspected STEMI cases for troponin values.
- ECG:
- NSTEMI vs STEMI:
- Elevation in troponin but differences in ECG changes.
- NSTEMI vs STEMI:
- ECG of UA/NSTEMI: No abnormalities, ST-segment depression, T wave inversion.
- Definition: “new horizontal or downsloping ST-depression ≥0.5 mm in two contiguous leads and/or new T wave inversion >1 mm in two contiguous leads with prominent R wave or R/S ratio >1”.
- ST-T wave changes can be seen diffusely or localize to region of ischemia.
- ST-T ECG changes often persistent in NSTEMI vs transient in UA.
- Absence of ST segment elevation or pathological Q waves.
- T-wave inversion can be normal variant in leads III, aVR, V1.
- Upsloping ST Depression is non-specific for myocardial ischemia.
- Greater degree of ST Depression is associated with worse prognosis.
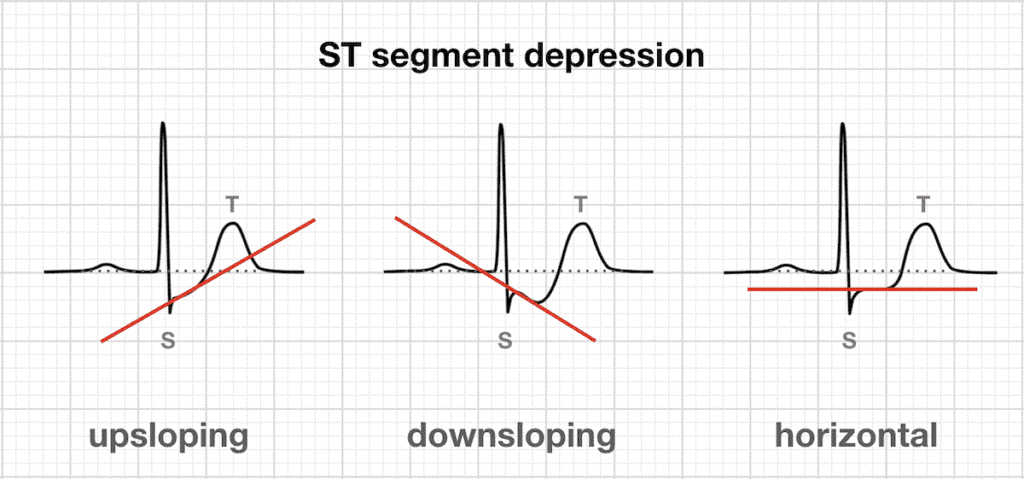
Image 1: Example of ST segment depression. Source: https://litfl.com/myocardial-ischaemia-ecg-library/
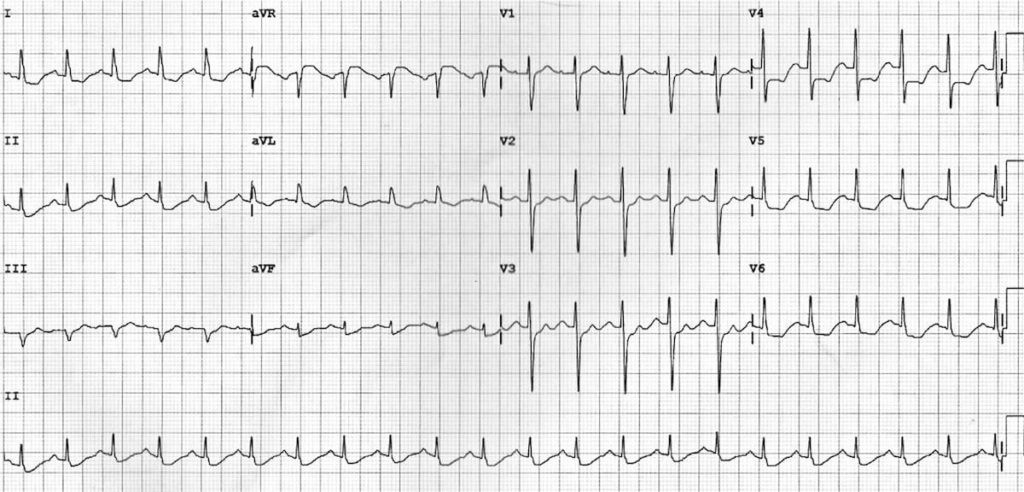
Image 2: 12 lead ECG showing ST segment depression. Source: https://litfl.com/myocardial-ischaemia-ecg-library/
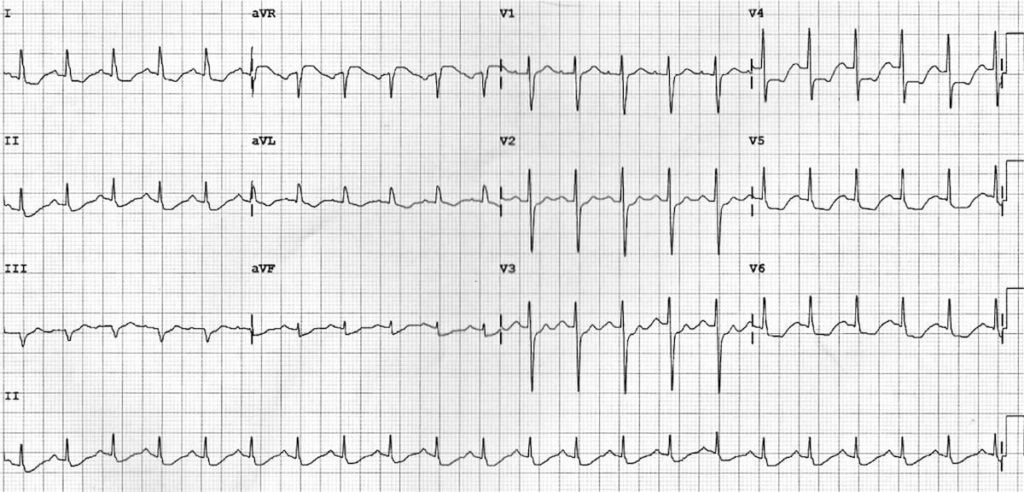
Image 3: New T wave inversion. Source: https://litfl.com/myocardial-ischaemia-ecg-library/
- ECG of STEMI: New ST-segment elevation at J point in 2 contiguous leads: ≥1 mm all leads:
- ≥2 anterior or inferior or posterior leads (NOTE 2 mm elevation anteriorly no longer threshold – in Vancouver at least).
- ST segment elevation differential includes:
- Acute myocardial ischemia.
- acute pericarditis, myocarditis.
- benign early repolarization.
- massive PE.
- Brugada-type patterns.
- Old MI and persistent ST segment elevation.
- Can also manifest as new LBBB or patients with a true posterior MI.
- Inferior wall ischemia (leads II, III, aVF) should prompt right sided leads for possible RV infarct.
- ST segment depression in inferior leads should also prompt posterior leads for possible posterior infarct.
- Note: Non-diagnostic ECGs are common. If suspicion for ACS high, repeat ECG at 20-30 min intervals.
- ECG features suggestive of prior MI:
- Abnormal Q waves.
Aside: Can also have imaging evidence of myocardial ischemia.
Diagnostic Algorithm:
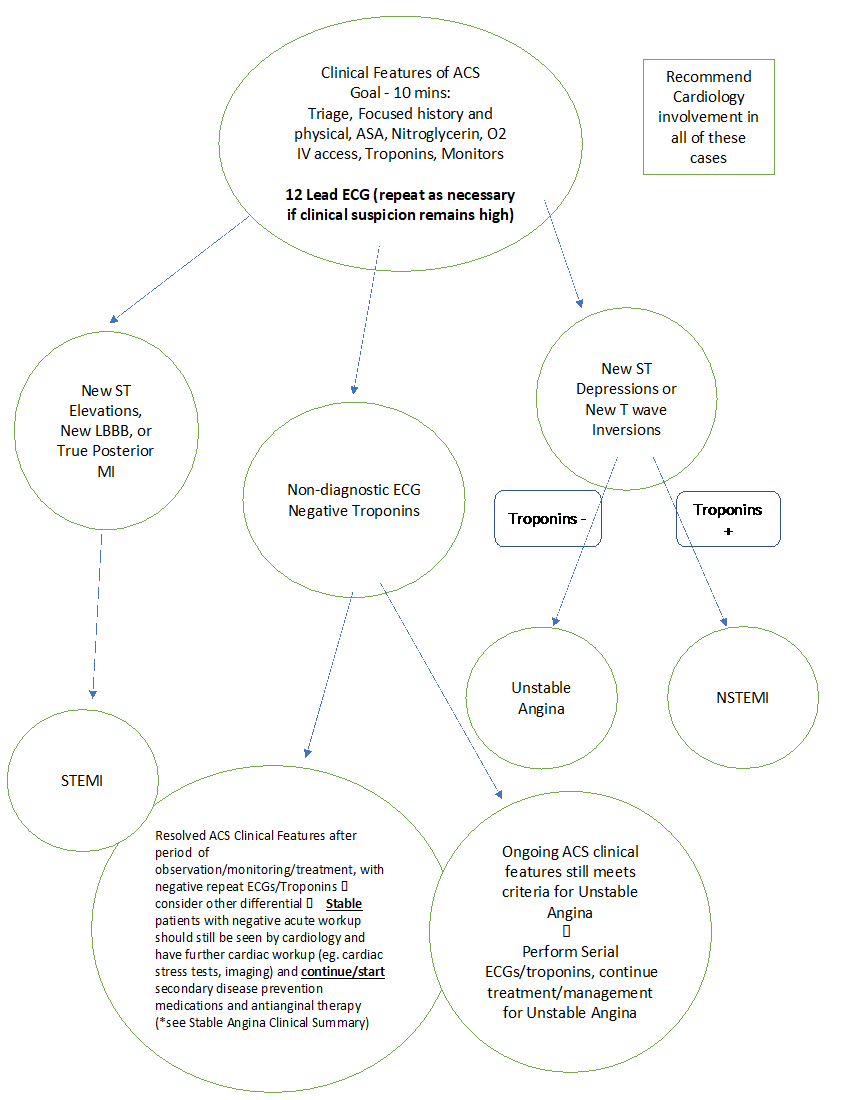
Figure 1: ACS Diagnostic Pathway.2,4, 6
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
The evidence for this article was taken from the most up to date literature which is peer reviewed for accuracy.
Related Information
Reference List
Hooton TM, Gupta K. Diagnosis of acute myocardial infarction. In: UpToDate, Post, TW (Ed), UpToDate, Waltham, MA, 2020.
Hooton TM, Gupta K. Initial evaluation and management of suspected acute coronary syndrome (myocardial infarction, unstable angina) in the emergency department. In: UpToDate, Post, TW (Ed), UpToDate, Waltham, MA, 2020.
Hooton TM, Gupta K. Acute coronary syndrome: Terminology and classification. In: UpToDate, Post, TW (Ed), UpToDate, Waltham, MA, 2020.
Hooton TM, Gupta K. Overview of the acute management of non-ST elevation acute coronary syndromes. In: UpToDate, Post, TW (Ed), UpToDate, Waltham, MA, 2020.
https://litfl.com/myocardial-ischaemia-ecg-library/
Barstow et al. Acute Coronary Syndrome: Diagnostic Evaluation. Am Fam Physician. 2017;95(3):170-177.
Appendix-Ischemic Pain Suspected Initial Management Orders
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jun 16, 2021
Visit our website at https://emergencycarebc.ca
COMMENTS (2)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.