Contrast Allergy – Treatment
Critical Care / Resuscitation, Toxicology
Context
- Contrast allergies are rare events, most commonly following intravascular use of contrast media, though can occur with other routes of administration.
- Most reactions are mild and self-limited; however, reactions can be life threatening.
- Reactions are either anaphylactoid or non-anaphylactoid (chemotoxic) in origin.
- Reactions can be acute or delayed; as well as allergic-like (anaphylactoid) or physiologic.
- Treatment is determined via clinical presentation and severity of reaction.
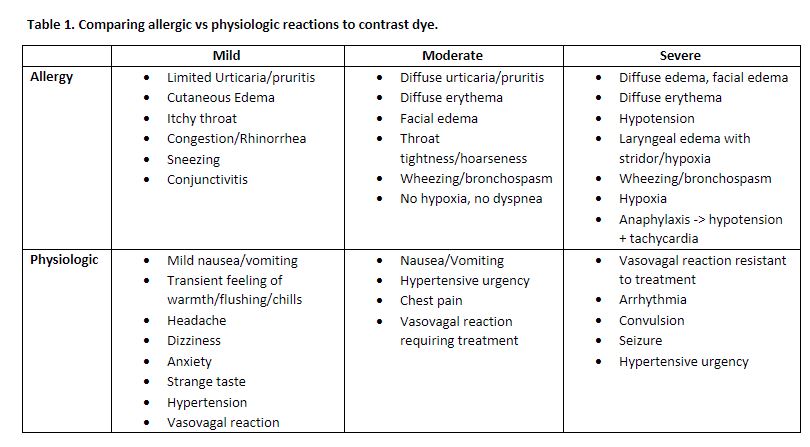
Signs and Symptoms
Created by Ella Barrett-Chan, MSI UBC 2023
Recommended Treatment
Delayed Reactions
- Reactions are typically self-limited and require only supportive care on an outpatient basis:
- Cutaneous symptoms – antihistamines, corticosteroids.
- Fever – antipyretics.
- Nausea – antiemetics.
- Hypotension – fluid resuscitation and observation 4-6 hours usually required.
- If symptoms are progressive, referral to consultation with an allergist or dermatologist indicated.
Acute Reactions
- A patient with acute onset of symptoms following administration from contrast should be presumed a contrast allergy unless otherwise explained.
- Stop contrast administration.
- Mild reactions: usually self-limited, but require observation for at least 30 minutes and until symptom resolution.
- Moderate or severe reactions: immediate therapy – obtain IV access and O2.
- Further treatment is determined by the clinical presentation, listed below.
Patient Unresponsive
- Securing of airway and resuscitation according to ACLS/PALS guidelines.
- Perform treatment protocols for a severe allergic-like contrast reaction.
Allergic-like Symptoms
Hypotension and Tachycardia
- Epinephrine – see below for dosage.
- Shock management – rapid fluid resuscitation.
- Adults: 1-2 L of NS IV.
- Infants, children & adolescents: 20 mL/kg over 5-10 mins (max of 0.5-1 L).
Bronchospasm
- Mild – ß-agonist inhaler (i.e. salbutamol) – 2 puffs (100 mcg/puff) via metered dose inhaler; repeat up to 3 times.
- Moderate to severe (or other organ system involvement) – epinephrine and adjunctive ß-agonist inhaler.
Laryngeal Edema
- Epinephrine.
Widespread Cutaneous Symptoms (i.e. edema, urticaria, erythema)
- Mild to moderate – H1 antihistamine (i.e. diphenhydramine)
- Adults: 25-50 mg IM or IV (PO can be considered if mild).
- Children: 1 mg/kg up (max 50 mg; PO can be considered if mild).
- Severe – epinephrine.
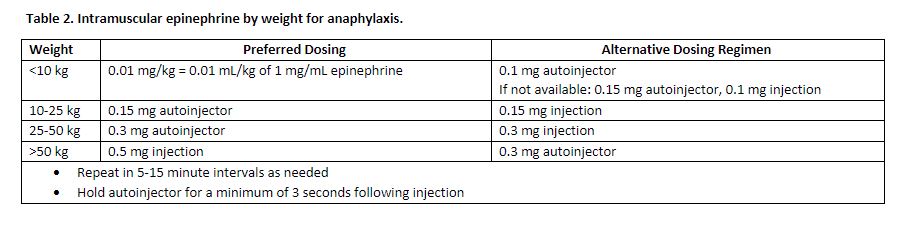
Notes on epinephrine dosage:
Created by Ella Barrett-Chan, MSI UBC 2023
Physiologic Symptoms
Hypotension and Bradycardia
- Initiate management of a vasovagal reaction
- Lie patient supine with legs elevated > 60 degrees
- If symptoms of end-organ dysfunction, initiation of rapid fluid resuscitation with 1-2L of NS IV
- Infants, children & adolescents should receive NS boluses of 20 mL/kg over 5-10 minutes, repeat as needed
- If not responsive to initial fluid bolus, administer atropine
- Adults: 0.6-1 mg IV every 3-5 minutes (maximum 3 mg: consider epinephrine infusion 1-4 mcg/min up to 20mcg/min)
- Infants, children, adolescents: 0.02 mg/kg IV (maximum 0.5 mg); can be repeated once 3-5 minutes after initial dose (maximum total dose = 1 mg)
Hypertension
- Monitor; self-limited pending urinary clearance of contrast (can be facilitated via IV/oral hydration)
- If hypertensive crisis (>200 mmHg SBP or >120 mmHg DBP)
- Labetalol IV 20 mg over 2 minutes; dose can be doubled every 10 minutes if further administration required
- Furosemide IV 20-40 mg over 2 minutes (given to increase clearance not reduce volume)
Seizures/Convulsions
- Turn patient on side to prevent aspiration and suction airway as required
- Slow administration of Lorazepam IV 2-4 mg (Careful > 4 mg: resp depression and hypotension)
Hypoglycemia
- If able to swallow: oral glucose – two sugar packets or 15 g glucose tablet/gel or ½ cup of juice.
- If unable to swallow and IV access available – 25 g (adults) or 2 mL/kg (children) D50W IV over 2 minutes; then D5W IV at 100 mL/hour.
- If no IV access available – Glucagon IM 1 mg (0.5 mg if <20 kg).
Cardiopulmonary Symptoms
- Initiate appropriate protocols for manifesting symptoms (i.e. chest pain, arrhythmia, pulmonary edema, etc).
Nausea and Vomiting
- If transient, supportive treatment; consider antiemetics if severe.
Criteria For Hospital Admission
- All patients with severe reactions should be admitted for observation.
- Admission should be considered for patients who are at risk of a biphasic response (i.e. do not respond promptly to IM epinephrine, required more than one dose of epinephrine, or received epinephrine after a >60 minute delay).
Criteria For Safe Discharge Home
- Mild to moderate reactions – observe until symptom resolution.
- All patients who have experienced an allergic-like contrast reaction should be referred for skin testing to identify future safe contrast alternatives and pre-medication requirements.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
References to primary studies lacking; however, extremely high congruency and well-established clinical guidelines from medical societies responsible for oversight of contrast administration worldwide.
Related Information
Reference List
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jun 04, 2021
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.