D-Dimer
Hematological / Oncological, Respiratory
Context
- Appropriate use of D-dimer can save hospital resources and patient exposure to CT radiation/contrast in working up PE and DVT.
- D dimer is a byproduct of blood clotting and breakdown process.
- High sensitivity but low specificity for PE or DVT in low-risk populations
- Always a “rule out” test – never used to “rule in” VTE.
- There are specific cases in which D-dimer can be helpful, and many in which it is useless or can potentially lead to patient harm through over investigation.
- There are many causes of D-dimer elevation other than VTE:
- Thromboembolism (ex. stroke, MI, intracardiac thrombus, DIC).
- Inflammation: infections, sepsis, COVID-19.
- Surgery/Trauma.
- Hepatic disease, renal disease.
- Malignancy.
- Vascular malformations, aortic dissection.
- Pregnancy.
When to use D-dimer
- PE/DVT on differential diagnosis but:
- PE unlikely based on Well’s Criteria for PE (<4.5).
- DVT unlikely based on Well’s Criteria for DVT (<2).
- In the above situations, if d-dimer is negative, PE/DVT is rule out. If positive, further investigation via imaging is required.
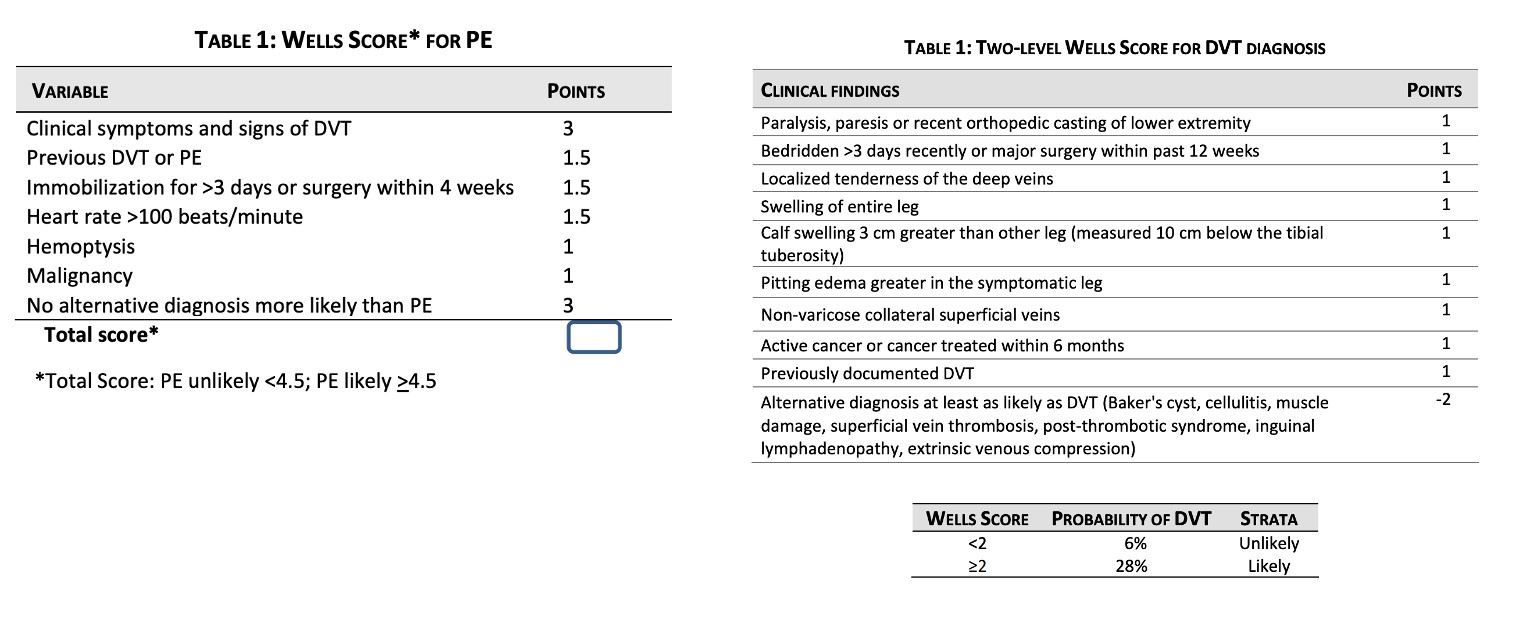
Table 1. Well’s Scores. Adapted from Thrombosis Canada DVT and PE guidelines (2021)
When NOT to use D-dimer
- PE on differential but:
- All PERC criteria are met – satisfactorily ruling out PE.
- Well’s score for PE is >4.5.
- Clinical suspicion is high enough for PE that CTPE or thoracic imaging will be ordered anyway.
- Patient is hypotensive/unstable with SBP<= 90.
- DVT is on differential but:
- Well’s score for DVT is ≥ 2.
- Clinical suspicion is high enough for DVT that compressive ultrasound will be ordered anyway.
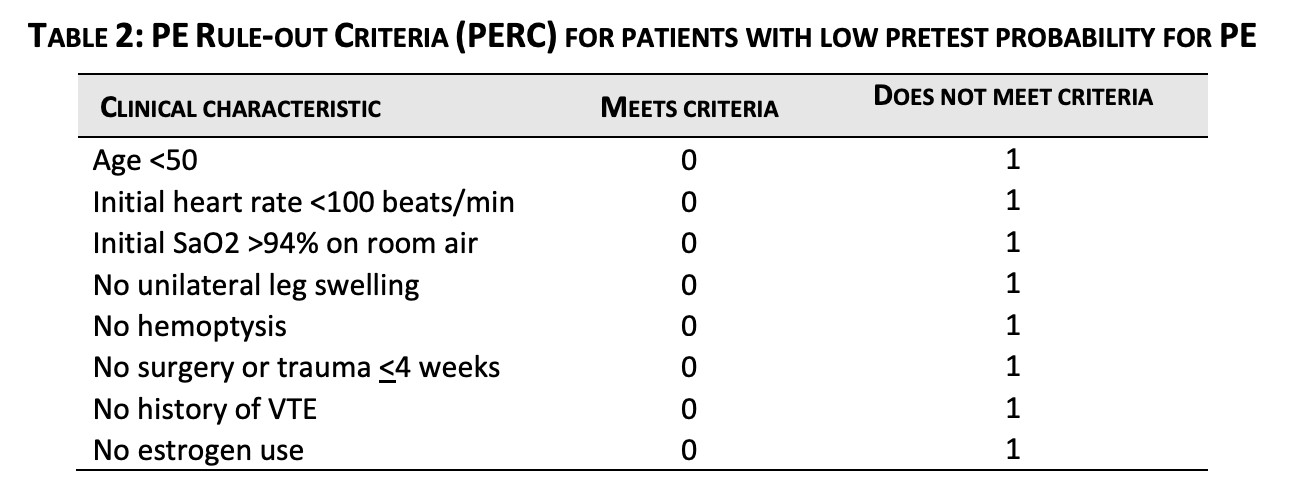
Table 2. Adapted from Thrombosis Canada Pulmonary Embolism Guidelines (2021)
Pearls
- Age adjustment for high sensitivity D-dimer increases the specificity of D-dimer testing for PE (evidence lacking for DVT).
- In patients >50, D dimer is negative if less than patient age multiplied by 10 – for example if 80-year-old patient, negative is <800 µg/L..
- If <50, cut off is <500 µg/L.
- There is mounting evidence for a 3-tiered Well’s score for PE and DVT modifying D-dimer cut-off based on pre-test probability to further reduce unnecessary imaging:
- PE: If low clinical probability (Wells score 0 to 4) and D-dimer <1000 µg/L, or moderate clinical probability (Wells score 4.5 to 6) and D-dimer <500 µg/L, PE can be ruled out.
- DVT: If low clinical probability (Wells score -2 to 0) and D-dimer <1000 µg/L, or moderate clinical probability (Wells score 1 to 2) and D-dimer <500 µg/L, DVT can be ruled out.
- Note: This idea has been cited in Thrombosis Canada guidelines as “safe” for both PE and DVT but has not yet implemented in their suggested algorithms for PE/DVT diagnosis.
- In patients >50, D dimer is negative if less than patient age multiplied by 10 – for example if 80-year-old patient, negative is <800 µg/L..
Pitfalls:
- Over-reliance on clinical decision tools
- Well’s score criteria for “alternative diagnosis more likely than PE” can change management in nearly all patients, which is entirely based on clinical judgement.
- Reflexive ordering of D-dimer without proper rationale to justify change in management based on results.
- There is insufficient evidence to support routine use of D-dimer in screening for aortic dissection.
- The use of D-dimer for DVT and PE has not been validated in pediatric populations.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
- The Well’s scores for DVT and for PE have high quality evidence as clinical decision-making tools which has been validated in numerous subsequent studies and meta-analyses.
- The 3-tiered approach for both adjusted-d-dimer DVT and PE diagnosis is moderate quality evidence based on excellent study design and magnitude of effect but lacks replication in subsequent trials.
Related Information
OTHER RELEVANT INFORMATION
-
-
Likelihood ratios/statistical analysis of clinical scoring systems combined with D-Dimers: http://blog.clinicalmonster.com/2020/02/28/working-up-pe-in-the-ed-negative-likelihood-ratios-and-fagan-nomograms/
Related Information
Reference List
Thrombosis Canada. (2021). Deep Vein Thrombosis: Diagnosis. https://thrombosiscanada.ca/wp-content/uploads/2021/07/2.-Deep-Vein-Thrombosis-Diagnosis_20July2021.pdf
Thrombosis Canada. (2021). Pulmonary Embolism: Diagnosis. https://thrombosiscanada.ca/wp-uploads/uploads/2021/11/4.-Pulmonary-Embolism-Diagnosis_14November2021.pdf
Kearon C, de Wit K, Parpia S, Schulman S, Afilalo M, Hirsch A, et al. Diagnosis of Pulmonary Embolism with d-Dimer Adjusted to Clinical Probability. New England Journal of Medicine. 2019 Nov 28;381(22):2125–34.
Kearon C, de Wit K, Parpia S, Schulman S, Spencer FA, Sharma S, et al. Diagnosis of deep vein thrombosis with D-dimer adjusted to clinical probability: prospective diagnostic management study. BMJ. 2022 Feb 15;376:e067378.
Related Information
OTHER RELEVANT INFORMATION
Thrombosis Canada DVT discharge sheet: https://thrombosiscanada.ca/wp-content/uploads/2016/05/M159-You-Have-a-DVT.pdf
Thrombosis Canada PE discharge sheet: https://thrombosiscanada.ca/wp-content/uploads/2016/10/M159-You-Have-a-PE_Oct2016.pdf
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Dec 16, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.