Diplopia
Ears, Eyes, Nose, and Throat
Context
- Diplopia is the perception of double vision.
- Diplopia is classified as either binocular, which resolves when the patient covers either eye or monocular, which persists when the non-affected eye is covered.
- Monocular diplopia indicates a problem intrinsic to the affected eye, whereas binocular diplopia indicates misalignment of the eyes.
- 85% of diplopia is binocular.
- Diplopia may be secondary to a relatively benign cause such as refractive error or indicate a serious underlying pathology such as a brainstem stroke, MS, brain tumours, or botulism.
- Monocular diplopia is almost never a neurologic problem and results from distortions to the light path in the affected eye. The most common causes include keratoconjunctivitis sicca (dry eyes), cataracts, corneal irregularity and rarely retinal irregularities.
- Binocular diplopia results from misalignment of the eyes and most commonly arises from CN VI, III or IV palsies, with other causes including oculomotor muscle dysfunction, systemic disease processes or CNS lesions.
Diagnostic Process
Recommendations
- Diplopia should be characterized as either: monocular or binocular, horizontal or vertical, acute or progressive, painful or painless, traumatic or non-traumatic and isolated or associated with other neurological signs.
- True sudden onset suggests an ischemic/vascular cause.
- Eye pain is associated with inflammation/infection
- Concerning neurological features include focal neurodeficits, headache, meningismus or fever
- Mandatory physical exam components include:
- Assessment of the 6 cardinal movements of gaze.
- Facial examination looking for ptosis, pupillary asymmetry (i.e mydriasis)
- Possible adjunctive investigations include:
- Fundoscopy for papilledema.
- Slit Lamp Examination
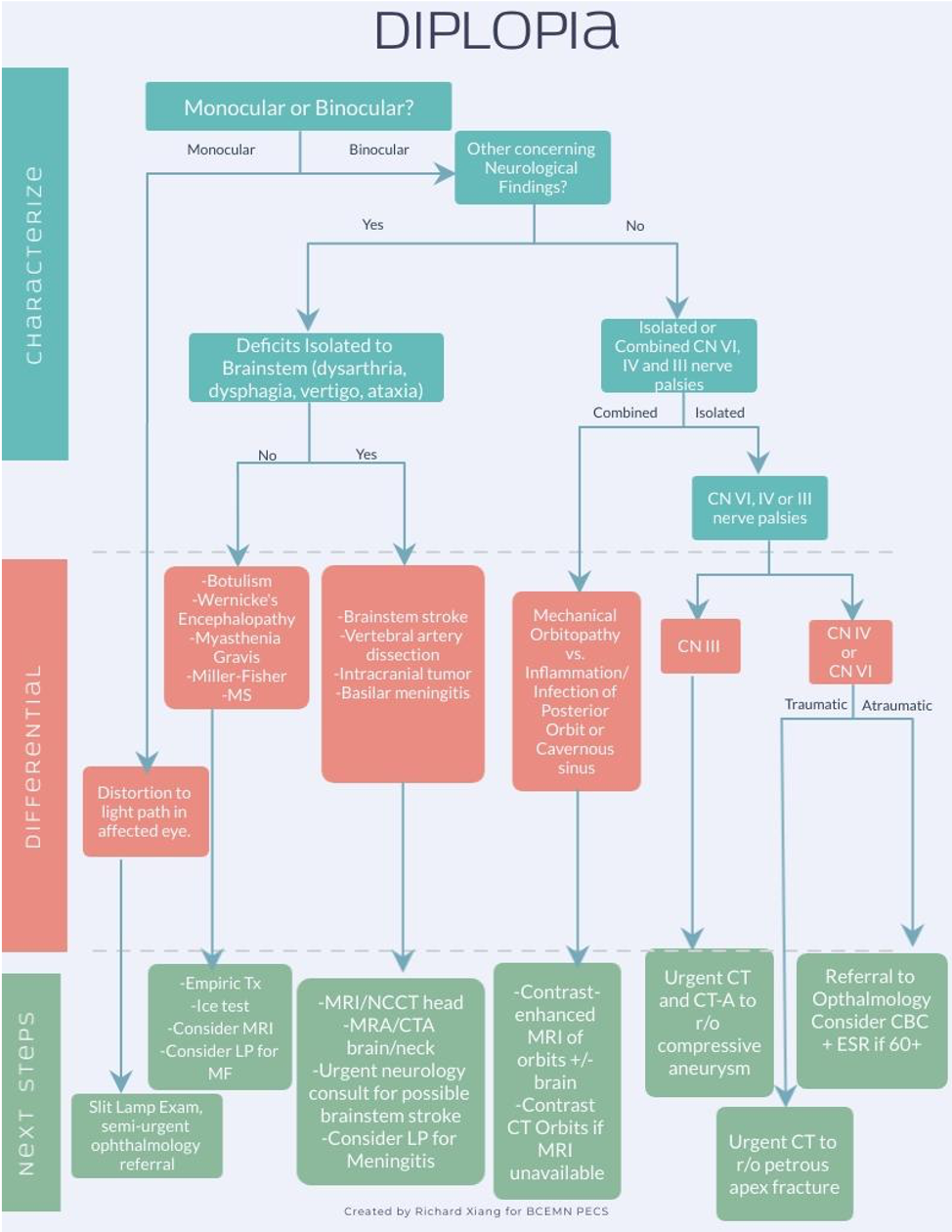
CLICK TO ENLARGE
Monocular Diplopia
- Monocular diplopia is commonly caused by keratoconjunctivitis sicca (dry eyes), cataracts, corneal irregularity and rarely retinal irregularities. After a slit lamp examination, patients can be referred to an ophthalmologist and discharged safely.
Binocular Diplopia
Concerning Neurological Deficits
- If neurological deficits are isolated to the brainstem (dysarthria, dysphagia, central vertigo), then assume stroke until proven otherwise. Activate your hospital’s stroke protocol and consult a neurologist for possible brainstem stroke.
- If diplopia is associated with neurological symptoms outside of the brainstem, consider work-up for other causes of diplopia discussed below.
Isolated CN VI, IV or III Palsies
CN III Palsy
- The eye is “down and out”, abducted and looking inferiorly. Usually presents with mydriasis and ptosis. Requires immediate CT and CTA to rule out a compressive aneurysm, most commonly at the junction of the posterior communicating and internal carotid arteries. Failure to identify a compressive aneurysm may lead to SAH and death.
- The absence of mydriasis (a.k.a “Rule of the Pupil”)is not a sensitive way to r/o a compressive aneurysm.
CN IV Palsy
- Vertical/torsional diplopia with near normal eye movements. Worst when looking down and toward the nose. Usually caused by decompensation of a congenital CN IV palsy, trauma or microangiopathic changes. Non-urgent referral to ophthalmologist is recommended.
CN VI Palsy
- Inability to abduct the affected eye, often with severe pain localized around the eye with the abduction defect. If this is an isolated, unilateral neurological finding with the presence of vascular risk factors, neuroimaging is typically unrevealing and non-urgent referral to an ophthalmologist is appropriate with spontaneous resolution of this palsy over 10-12 weeks. If the deficit lasts beyond 3 months, an urgent MRI brain should be obtained to rule out non-microvascular causes.
- An isolated CN VI palsy in a child requires an urgent MRI of the brain because nerve compression is the most common cause of an isolated CN VI palsy in the pediatric population.
- Bilateral CN VI palsies suggest more ominous etiologies such as ICH, subdural hematoma and brainstem infarcts.
- If ocular motility appears to be from multiple ocular motor nerves, it is reasonable to order a semi-urgent MRI of the cavernous sinuses/orbits with semi-urgent referral to Ophthalmology/Neurology. In the absence of any other neurological signs, it is safe for the patient to wait to see a specialist who is able to do a complete ocular alignment and motility workup.
Traumatic Diplopia
- Obtain NCCT Head and Orbits to rule out petrous apex fracture.
Mechanical Orbitopathy/Myositis
- Signs include proptosis, periorbital swelling, edema, conjunctival hyperemia or unilateral palpebral swelling.
- Causes include:
- Graves orbitopathy causing enlargement/fibrosis of extraocular muscles. (Typically have previous diagnosis of hyperthyroidism and present with eyelid retraction, chemosis, conjunctival injection and proptosis)
- Traumatic/Inflammatory/Neoplastic Mass Effect
- Obtain a Contrast-Enhanced MRI of the orbits +/- brain.
Cavernous Sinus Infection/Mass/Vasculitis
- Can affect CN III, IV and VI simultaneously and typically affects CN VI first (orbital apex syndrome).
- Causes:
- Carotid-cavernosus fistula
- Infectious/Inflammatory: GCA, Tolosa Hunt syndrome, Herpes Zoster Ophthalmicus
- Tumor/Invasive Dx: (Lymphoma, Sarcoidosis)
- Iatrogenic: Intravascular injection or diffusion of anesthetic into pterygoid venous plexus.
Other Causes
Myasthenia Gravis
- 60% present with ptosis/diplopia and fluctuating muscle weakness that worsens with eye movements in any cardinal direction of gaze. Associated symptoms include proximal muscle weakness, SOB or difficulty swallowing If suspected, semi-urgent referral to neurology is recommended, without need for CT scan.
- Ice Test – Apply ice to patient’s closed eye and hold for 5 minutes, improvements in ptosis/diplopia suggest reversal of acetylcholine receptor blockade.
Wernicke’s Encephalopathy
- Diplopia associated with ataxia and altered mental status in a patient with chronic ETOH use or bariatric surgery. If suspicion for Wernicke’s Encephalopathy, treat empirically with IV thiamine infusion.
Botulism
- Gradual onset of dysarthria, dysphagia and double vision with foodborne exposure. May also have autonomic dysreflexia or pupillary dysfunction. Hospitalize immediately and monitor for any signs of respiratory compromise. Can consider intubation if the airway is at risk.
Multiple Sclerosis
- Internuclear Ophthalmoplegia, (inability to adduct the eye with nystagmus of the contralateral eye), along with optic neuritis (blurred vision and eye pain). Obtain MRI imaging and consult neurology.
Giant Cell Arteritis
- Uncommon cause of diplopia, associated with 2.7% of isolated sixth nerve palsy with no other systemic symptoms or signs. Obtain CBC and ESR in all patients 60+ with recent onset of diplopia. Urgent consultation to ophthalmology, as the patient may require temporal artery biopsy and/or initiation of high-dose systemic corticosteroids.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Recommendation: No initial imaging is necessary for isolated CN VI palsy.
Low Quality. Alternate conclusions reached by different studies:
- 2004 retrospective study on 93 isolated, non-traumatic CN VI palsy, with the majority of patients experiencing spontaneous, complete resolution without MRI. (Incidence, associations, and evaluation of sixth nerve palsy using a population-based method). (Patel et al 2004).
- 2004 prospective study with 4/23 patients with isolated abducens palsy having an alternative dx to microischemia that would change acute management/long-term prognosis. (Acute ocular motor mononeuropathies: prospective study of the roles of neuroimaging and clinical assessment)
- 2011 prospective study found only 1/93 had a causative lesion identifiable on MRI, with no change in management for any patient. (Neuroimaging and acute ocular motor mononeuropathies: a prospective study). (Murchison et al. 2011)
- 2013 prospective study with 62 patients with isolated abducens palsy, with 12/62 due to non-microvascular causes that would have been detected on MRI and would change management.
Recommendation: The rule of the pupil (Absence of mydriasis in CN III palsy to rule out compressive etiology of third nerve palsy) should not guide the decision to obtain CTA. Moderate Quality
- Retrospective chart review of 145 patients with acquired third nerve palsy. Of those with compressive third nerve palsies (25), 64% (16) had pupillary involvement (mydriasis)(Fang et al. 2017).
- Case report documenting a 79 y/o male with ptosis and binocular diplopia consistent with a CN III palsy but no pupillary involvement. Eventually diagnosed with myasthenia gravis after the palsy failed to resolve after 3 months. Granted, this is unrelated to compressive third nerve palsies, however it provides very weak evidence that pupillary sparing may not be sufficient to avoid further imaging, therefore may require imaging regardless (Wood 2010).
Related Information
Reference List
Relevant Resources

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Mar 05, 2021
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.