Drowning
Critical Care / Resuscitation, Environmental Injuries / Exposures, Pediatrics, Respiratory, Trauma
First 5 Minutes
- Primary objective is to reverse hypoxia by providing adequate oxygenation and ventilation.
- Hypothermia is frequently linked to drowning and is a protective mechanism allowing for survival in prolonged submersions. Therefore, if cardiac arrest occurs, prolong resuscitative measures for longer than usual and attempt to normalize core body temperature as rapidly as possible before ceasing resuscitative efforts.
- In initially asymptomatic patients, symptoms can develop any time within the first 8 hours after a drowning event.
- Consider suicidality or medical condition as possible precipitating factors.
Context
- Drowning is a leading cause of accidental death worldwide and is a prominent cause of pediatric deaths.
- Fluid aspiration causes loss of surfactant leading to alveolar collapse, pulmonary edema and V/Q mismatch all resulting in hypoxemia.
- Cardiac arrest ultimately occurs due to hypoxemia and is typically preceded by bradycardia followed by PEA or asystole, however ventricular dysrhythmia can occur with cold water submersions.
- Fresh vs. saltwater has no clinical significance.
Diagnostic Process
Drowning is primarily a clinical diagnosis based on history of events.
Work-Up
- CXR, ECG.
- ABG.
- +/- CT head and c-spine if trauma suspected.
- Labs: CBC, Lytes, Bun, Cr, glucose, troponin, coagulation panel, urinalysis, CK, +/- EtOH levels; +/- toxicologic studies.
CLINICAL FEATURES
Pulmonary
- Hypoxemia due to fluid aspiration.
- Tachypnea and dyspnea.
- Rhonchi, rales and wheezes.
- Pulmonary edema.
Neurologic
- Altered level of consciousness.
- Myoclonic jerks or seizure activity.
- Comatose patients can have non-convulsive status. epilepticus that can only be seen on EEG.
Cardiovascular
- Hypoxemia and hypothermia can lead to cardiac dysrhythmias including sinus tachy/bradycardia, atrial fibrillation, PEA, and asystole.
- Cold water swimming and diving can induce fatal dysrhythmias in patients with underlying prolonged QT syndrome.
- ST-segment changes occur a result of takotsubo cardiomyopathy, coronary artery spasm, hypothermia or hypoxia.
- Rarely due to myocardial ischemia.
- Hypovolemia and hypotension caused by “cold diuresis” – blood is redirected to core organs causing central volume receptors to sense fluid overload causing a decrease in the production of antidiuretic hormone and an increase in urine production.
Metabolic
- Respiratory/metabolic acidosis.
Recommended Treatment
Manage ABC’s and clear c-spine.
Airway
- Intubate if:
- GCS <8 or unable to protect airways.
- Hypoxemia or hypercapnia on ABG despite high flow O2 (PaO2 < 60, PaCO2 > 50).
- Place OG/NG tube to relieve gastric distension.
- Supraglottic airways decreased odds of overall survival compared to intubation.
- Otherwise high flow O2 or CPAP if inadequate tidal volumes.
Breathing
- Maintain SpO2 >94%.
- If intubation is required, set ventilator to lung protective settings.
- Tidal volume 6-8 ml/kg of ideal body weight, plateau pressure <30mmHg, and increased PEEP.
- Permissive hypercapnia should be avoided if there is concern for hypoxic-ischemic brain injury.
- Other interventions to improve ventilation include placing patient in prone position, using bronchodilators to treat bronchospasms and administering inhaled nitric oxide.
Circulation
- For Grade 6: Continue resuscitation with ACLS protocol until the patient reaches a temperature between 32 – 35 degrees and asystole has been present for >20 minutes.
- If conventional CPR is not adequate, ECMO may be a salvage option where available on a case-by-case basis.
Neurologic
- Raise head of bed to 30° (if normotensive).
- Maintain MAP of 100mmHg for cerebral perfusion.
- Treat seizure activity with benzodiazepines.
Hypothermia
- Rewarming goal: 0.5℃/hr until 35℃ is reached, do not warm above 32-35 once ROSC is achieved for at least 12-24hrs.
- Passive Rewarming can be achieved by removing wet clothes, and insulating with blankets.
- Active Rewarming can be achieved with forced air warmers, warmed IVFs, and warmed humidified inspired gases, and ECMO.
- Once ABC’s addressed, treat hypotension with IV crystalloid fluids: 10cc/kg boluses in pediatrics.
- If hypotension is refractory to fluids, initiate a vasopressor infusion with epinephrine and arrange for echocardiogram and/or pulmonary artery catheterization to assess for etiologies.
- Only initiate broad-spectrum antibiotics if submersion occurred in heavily contaminated water.
- There is no role for glucocorticoids, exogenous surfactant, or barbiturates.
- Evaluate for additional injuries with appropriate imaging.
- Consider and treat precipitating factors of drowning – trauma, spinal cord injury, seizure, MI, arrhythmia, toxins, syncope, hypoglycemia.
Criteria For Hospital Admission
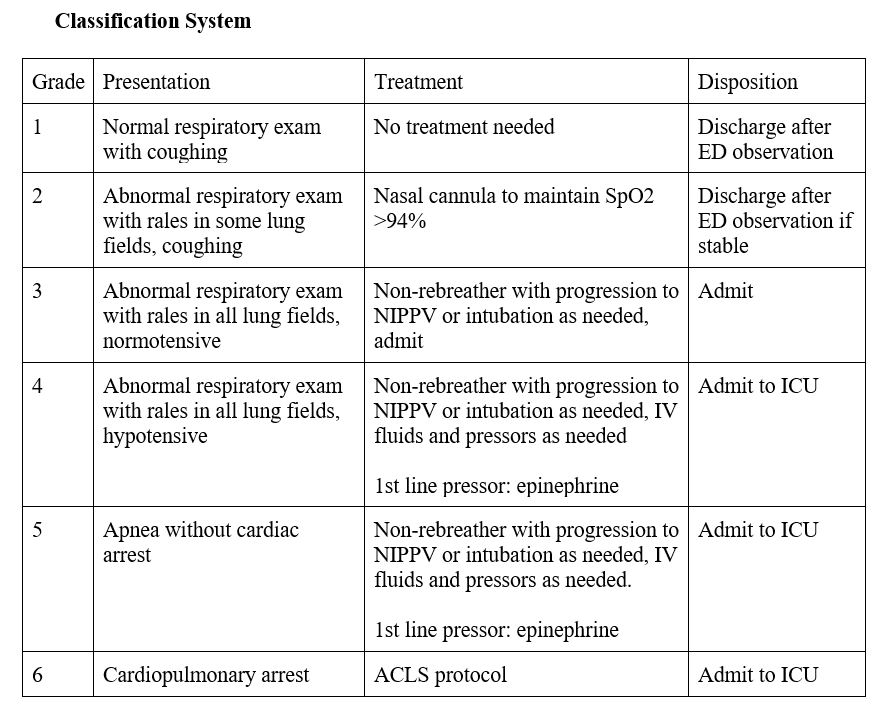
Admit all patients in Grade 3-6 to ICU.
Criteria For Transfer To Another Facility
- Consider transport to an ECMO center in patients with core temperature < 28°C, cardiac instability, BP < 90 mmHg or ventricular arrhythmias.
- If intubation required, transfer to facility with ICU once stabilized.
Criteria For Close Observation And/or Consult
- Any patient with dyspnea or cough with normal SpO2 (Grade 1-2) must be observed for a minimum of 8 hours.
- Can be discharged if after observation if: normal mental status, SpO2 >95% on room air, normal CXR and respiratory.
Criteria For Safe Discharge Home
Asymptomatic individuals may be discharged home under the supervision of an adult provided they did not develop any respiratory symptoms or impairment, have full recollection of the submersion, and normal SpO2 and vitals.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Recommendations based on clinical guidelines informed by a large range of studies, high-quality systematic reviews, and high-quality evidence from emergency medicine textbooks.
Related Information
OTHER RELEVANT INFORMATION
Drowned Airway Algorithm https://emcrit.org/pulmcrit/drowned-airway-algorithm/
Pediatric Drowning and Hypothermia
https://emergencymedicinecases.com/pediatric-drowning-hypothermia/
Approach to Drowning https://www.pedscases.com/approach-drowning
Reference List
Szpilman D, Morgan PJ. Management for the drowning patient. Chest. 2021;159(4):1473-1483.
https://doi.org/10.1016/j.chest.2020.10.007
Cico S, Quan L. Drowning. In: Tintinalli JE, Ma O, Yealy DM, Meckler GD, Stapczynski J, Cline DM, Thomas SH, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 9th ed. McGraw Hill; 2020:1-7. Accessed December 6, 2023.
https://accessmedicine.mhmedical.com/content.aspx?bookid=2353§ionid=220747025
Szpilman D, Sempsrott J, Schmidt A. Drowning. BMJ Best Practice. Updated November 15, 2023. Accessed December 6, 2023.
https://bestpractice.bmj.com/topics/en-gb/657
Pellegrino F, Raffaldi I, Rossi R, De Vito B, Pagano M, Garelli D, et al. Epidemiology, clinical aspects, and management of pediatric drowning. Ital J Pediatr. 2023;49(1):74.
https://doi.org/10.1186/s13052-023-01464-1
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated May 07, 2025
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.