Electrical Injuries
Critical Care / Resuscitation, Environmental Injuries / Exposures, Trauma
First 5 Minutes
Skin findings often significantly underestimate the degree of internal injury.
Context
3 types of electrical injuries: high voltage (≥1000V), low voltage (<1000V) and electric arc.
In electric arcs there is no passage of current through body tissues. There are 2 types of current:
- AC current is used in standard household electricity.
- DC current is used in batteries.
Exposure to AC currents can induce tetany causing prolonged exposure to electrical sources, respiratory apnea and ventricular fibrillation.
Both types of current can cause severe blunt force trauma through blast forces.
Injuries involve direct tissue damage from electricity, tissue damage from thermal energy, and mechanical injury from trauma.
Diagnostic Process
- Cardiac arrhythmias are common with atrial fibrillation being the most common. Other arrhythmias include sinus tachycardia, new right bundle branch blocks, AV conduction blocks, PVCs and QT-prolongation.
- Fatalities are often due to asystole and ventricular fibrillation.
- Respiratory arrest caused by tetanic contractions of thoracic muscles, injury to CNS or cardiopulmonary arrest secondary to ventricular fibrillation or asystole.
- Neurological findings include transient loss of consciousness, seizures, and focal neurological deficits – quadriplegia, hemiplegia, visual disturbances and paresthesias.
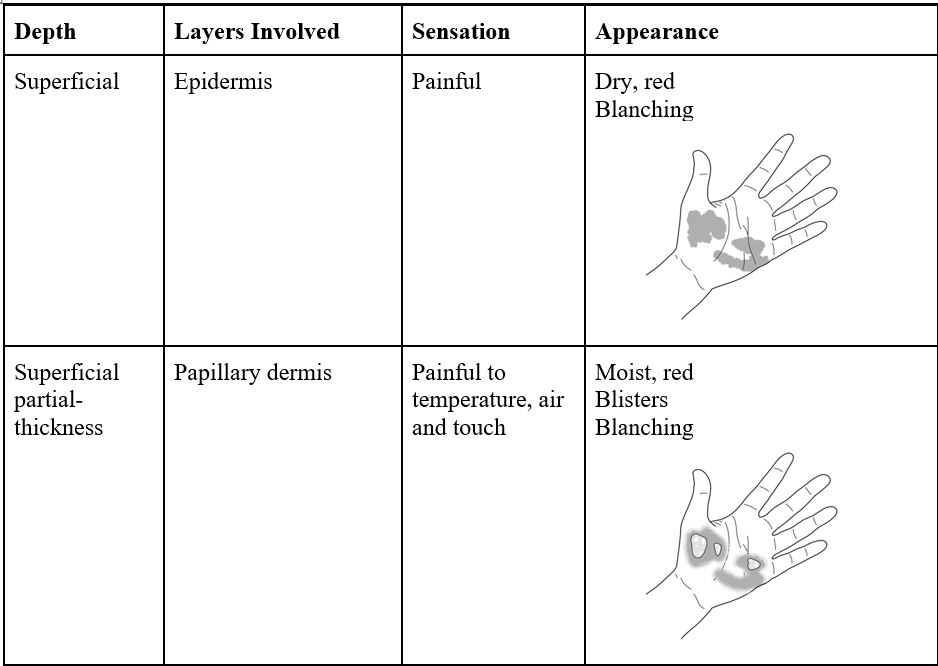
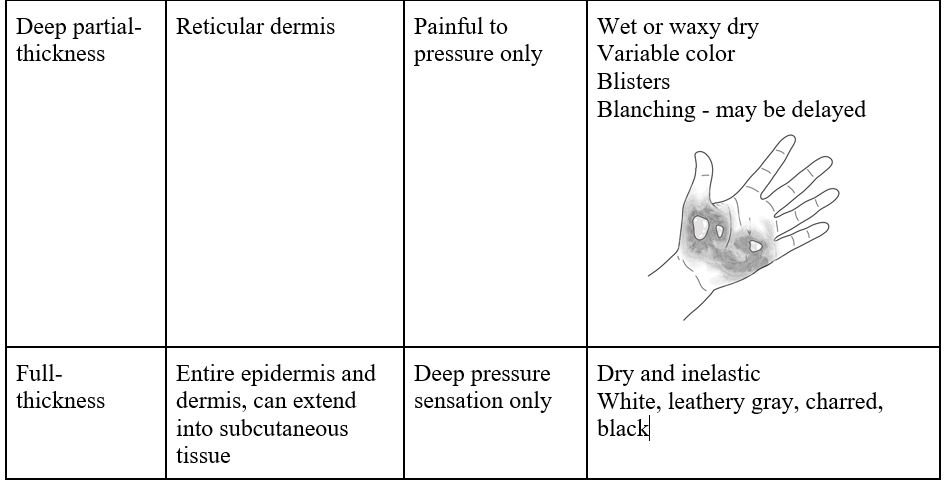
- Cutaneous Burns – determine depth of burns and TBSA.
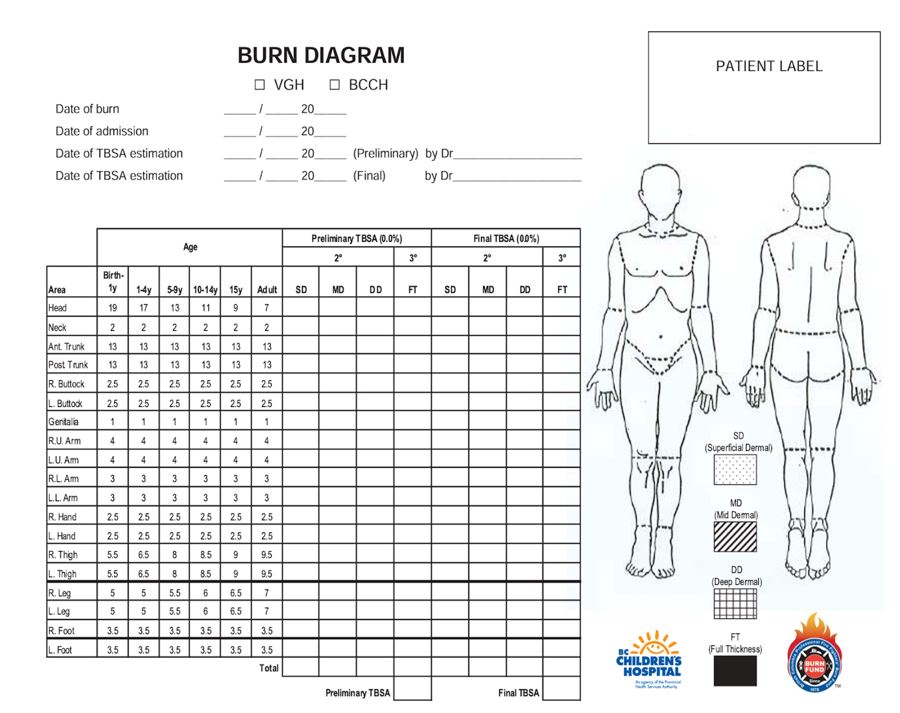
Pediatric burn diagram
Accessed from http://www.phsa.ca/health-professionals/clinical-resources/trauma/burns
Major Burn Criteria:
- ≥ 20% TBSA partial +/- full thickness burns, any age.
- ≥10% TBSA partial +/- full thickness burns if ≥65 years old.
- Burns to hands, feet, face, genitalia, or joints.
- Full thickness burns ≥5% TBSA, any age.
- Electrical burns – direct contact with high voltage source.
- Chemical Burns.
- Inhalation injury.
- Any burn with associated major trauma.
Assess for compartment syndrome, rhabdomyolysis, fractures and dislocations secondary to falls or tetany.
Have a high index of suspicion for GI vascular injuries and abdominal compartment syndrome.
Assess for ocular injuries to the cornea, and for uveitis, retinal detachment, macular edema, optic nerve damage, and intraocular bleeding.
Damage to the tympanic membranes is also common.
Investigations
- ECG.
- CBC, BMP, urinalysis, LFTs, coagulation panel, CK.
- +/- relevant imaging.
- Neuroimaging for patients with altered mental status, coma, or focal neurological deficits.
Recommended Treatment
Follow ACLS and ATLS protocols.
- There will often be return of spontaneous cardiac activity with ongoing respiratory arrest, therefore ensure adequate ventilation and oxygenation.
Early consultation with burn physician via Patient Transfer Network.
For burns meeting Major Burn criteria: Major Burns Trauma: Emergency Care BC.
- Initiate fluid resuscitation with crystalloids starting at 3cc/kg/%TBSA in the first 24hrs with first 50% given within 8 hours post-burn.
- Aim for a urine output of 50-100cc/hr.
- No evidence for use of diuretics to achieve target urine output.
- Consider escharotomy for full-thickness circumferential burns (in discussion with Burn Physician).
For burns not meeting Major Burn Criteria:
- Clean with saline soaked sterile gauze and cover with sterile dressings.
- Cool burns, but avoid inducing hypothermia.
- Topical dressing with silver for antimicrobial activity.
- Tetanus as needed.
- There is no role for prophylactic systemic antibiotic therapy.
Rhabdomyolysis: IV crystalloid fluid to maintain a urine output of ≥1cc/kg/hr.
Manage fractures and dislocations appropriately.
Pediatric Considerations
- Oral burns are seen in the pediatric population due to sucking/chewing on electrical cords.
- There is a risk of delayed hemorrhage from the labial artery.
- Admit for IV hydration, pain control and plastics evaluation if there is significant oral damage.
- If damage is confined to oral commissure discharge with follow-up with ENT or plastic surgery and education on serious delayed bleeding.
Criteria For Hospital Admission
All high-voltage electrical injuries should be admitted.
Additionally, hospital admission is indicated for any major burns, loss of consciousness, persistent neurological deficits, documented arrhythmias, hypotension, myoglobinuria or rhabdomyolysis, and pregnancy.
Criteria For Transfer To Another Facility
Burn Centre referral for burns meeting Major Burn criteria, plus all high-voltage or lightning injuries.
Criteria For Close Observation And/or Consult
Low-voltage electrical injuries should be monitored for 6 hrs.
Criteria For Safe Discharge Home
Low-voltage electrical injuries can be discharged home after 6hrs of monitoring if there are no ECG changes and patients have a normal physical exam.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Recommendations made based on high quality emergency medicine textbooks. However, there are limited studies which lack systemic methodology.
Related Information
OTHER RELEVANT INFORMATION
-
First 8 Hours Post Burn Adult Major Burns Clinical Practice Guidelines
Major Burn – Initial 24 hours Fluid Resuscitation Orders for Adults
Burn Resuscitation Protocol Pediatrics – Initial 48hrs
Severe Pediatric Burn Critical Care Orders
Core EM Electric and Lightning Injuries:
https://coreem.net/podcast/episode-1-0-electrical-and-lightning-injuries/
CanadiEM: https://canadiem.org/crackcast-episode-142-electrical-lightning-injuries/
BC Burn Centers:
Vancouver General Hospital
Royal Jubilee Hospital
BC Children’s Hospital ( <16 years old)
Patient Transfer Network: (604) 215-5911 or Toll Free 1-866-233-2337
Reference List
Jeschke MG, van Baar ME, Choudhry MA, Chung KK, Gibran NS, Logsetty S. Burn Injury. Nat Rev Dis Primers. 2020; 6(11): 1-20.
https://doi.org/10.1038/s41572-020-0145-5
Dheansa B, Hagiga A. Electrical injuries. BMJ Best Practices. Updated November 22, 2023. Accessed December 11, 2023.
https://bestpractice.bmj.com/topics/en-gb/655
Bailey C. Electrical and lightning injuries. In: Tintinalli JE, Mao O, Yealy DM, Meckler GD, Stapcynski J, Cline DM, Thomas SH, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 9th ed. McGraw Hill; 2020: 6-9. Accessed December 11, 2023.
https://accessmedicine.mhmedical.com/content.aspx?bookid=2353§ionid=220751208
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Dec 15, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.