Evaluation of Facial Trauma – Diagnosis
Cardinal Presentations / Presenting Problems, Ears, Eyes, Nose, and Throat, Trauma
Context
- The most common facial fractures include those to the nasal bone and mandible.
- Consider intimate partner violence and non-accidental trauma in every patient.
Diagnostic Process
Primary Survey
- Unless the facial injuries affect the ABCs, evaluate facial trauma during the secondary survey.
- Airway:
- Airway assessment and, if indicated, airway management are central in facial trauma.
- Assess for massive hemorrhage into the mouth and mechanical distortion from fractures or hematomas.
- Intubation is often necessary in patients with severe facial trauma.
- If active oral bleeding, consider double suctioning with an assistant during intubation.
- If significant distortion exists, a laryngeal mask airway may not form an effective seal. Furthermore, in this case, an awake fiberoptic intubation may increase first-attempt success.
- Mandibular fractures might make intubation easier.
- Be prepared for emergent cricothyroidotomy.
- C-spine:
- Have a low threshold for placing a collar—especially in the presence of severe facial fractures.
- Circulation:
- Life-threatening facial hemorrhage is rare; most bleeds can be safely managed during the secondary survey. If significant, control with direct compression, packing, or arterial ligation if the vessel can be visualized.
Secondary Survey
- Obtain an AMPLET history.
- The mechanism of injury predicts the severity of facial fractures and associated injuries (e.g., c-spine trauma).
- Four key questions:
- “How is your vision?”
- “Does any part of your face feel numb?”
- “Does your bite feel normal?”
- “Does your voice sound normal?”
- Systematically inspect the face from the front, superior, inferior, and sides for swelling, erythema, contusions, abrasions, lacerations, penetrations, asymmetry, and deformity. Then, palpate the entire face, including the orbital rims and bones overlying the sinuses, for tenderness, step-off deformities, instability, and crepitus. Remember to examine inside the mouth. See table 1 for clinical features of facial trauma and associated injuries.
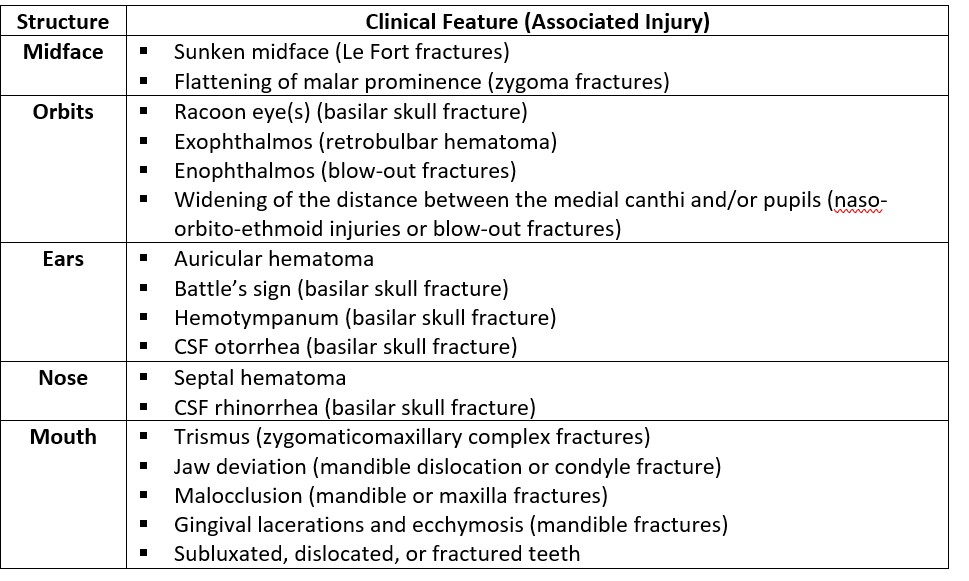
Table 1. Clinical Features of Facial Trauma
- Perform special tests as clinically indicated (see table 2).
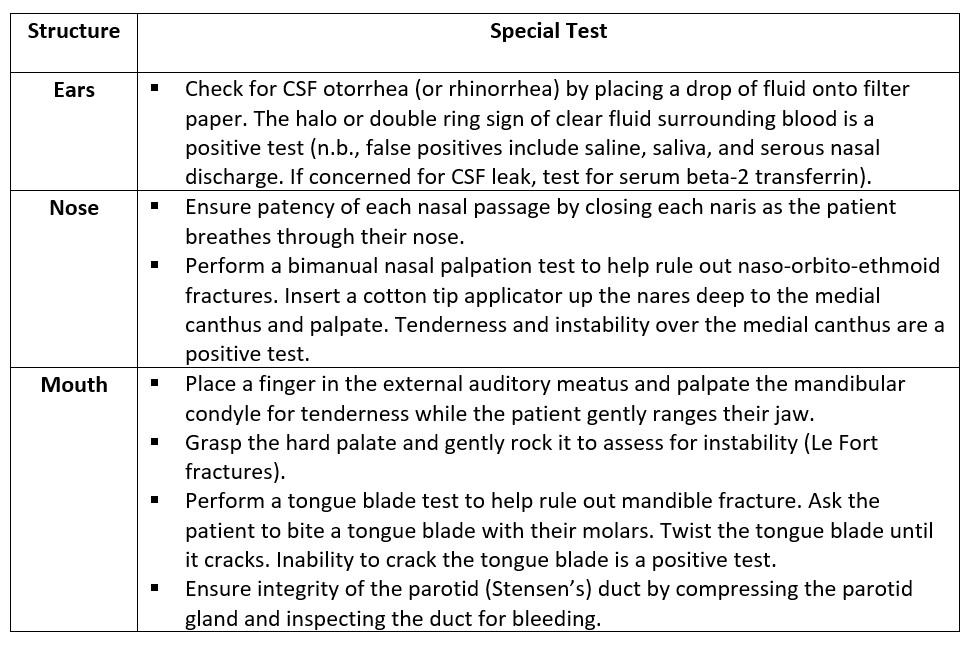
Table 2. Select Tests in the Evaluation of Facial Trauma
- If clinically indicated, perform a complete eye exam from front to back, including visual acuity, visual fields, extraocular movements, pupil shape and reactivity, intraocular pressure (in the absence of suspected globe rupture), fundoscopy, and slit lamp exam with fluorescein. Examine early on before the lids swell (use retractors if necessary). If no visual acuity, document perception of colours or light. Further evaluation of ocular trauma is beyond the scope of this PECS.
- Examine the cranial nerves.
Imaging
- The diagnostic imaging modality of choice for facial trauma is a non-contrast CT scan. The specific study depends on the level of injury:
- Frontal bone: head CT
- Can miss some facial fractures if only use this study.
- Midface and orbits: facial CT
- Patient positioning during image acquisition requires c-spine clearance.
- Mandible: mandible CT
- Frontal bone: head CT
- If clinically indicated, obtain multiple views (e.g., facial CT with mandibular views).
- Indications for imaging include, but are not limited to:
- Severe trauma.
- Altered mental status.
- Penetrating injuries (e.g., metallic foreign bodies.)
- Positive physical exam findings (e.g., deformity, swelling, ecchymosis, lacerations, hemorrhage, malocclusion, etc.)
- Radiographs can be used as an initial test if CT is unavailable, or the patient is at low risk.
- Incorporate the following decision rules for head and c-spine trauma as clinically indicated:
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
This resource is based on high quality evidence from the emergency medicine literature and academic texts. Facial CT +/- mandibular CT have high sensitivity and specificity for diagnosing facial trauma.
Related Information
Reference List
Hedayati T, Amin DP. Trauma to the Face. In: Tintinalli JE, Ma O, Yealy DM, Meckler GD, Stapczynski J, Cline DM, Thomas SH. eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 9e. McGraw Hill; 2020. Accessed August 17, 2022. https://accessmedicine.mhmedical.com/content.aspx?bookid=2353§ionid=222323488
Mayersak RJ. Facial Trauma. In: Walls RM, Hockberger RS, Gausche-Hill M, Erickson TB, Wilcox SR. eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice, 10e. Elsevier; 2023. Accessed August 17, 2022. https://www.clinicalkey.com/#!/content/book/3-s2.0-B9780323757898000347
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Oct 22, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.