Frostbite
Environmental Injuries / Exposures, Inflammatory
Context
- Military personnel, industrial workers, homeless populations, and recreational winter enthusiasts are most affected.
- Risk factors include alcohol consumption, smoking, homelessness, mental health disorders, inadequate protection, previous cold injury, polypharmacy, and working with equipment that uses NO2 or CO2.
- Causes dermatological, soft tissue, and vascular damage.
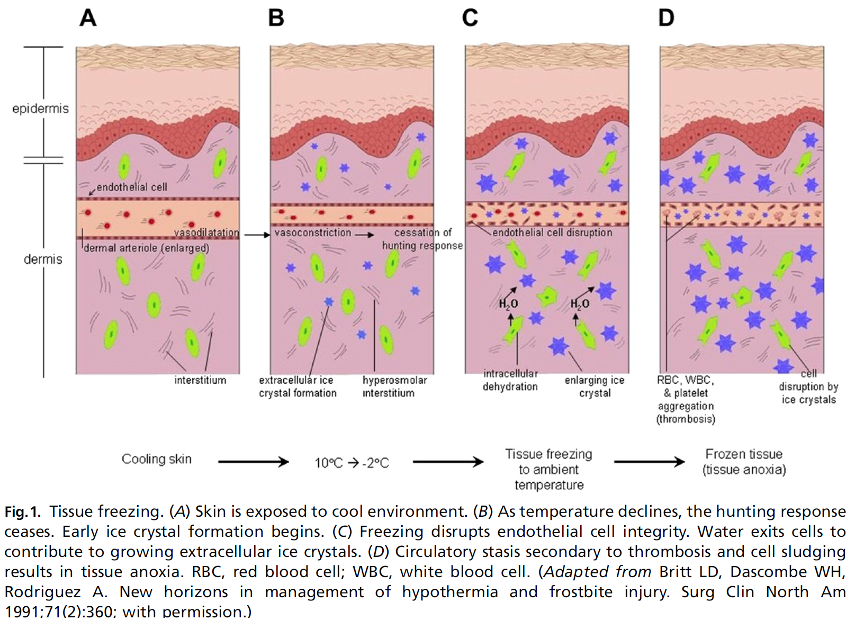
- Pathologic changes can be divided into:
- Direct cellular injury (e.g. ice crystal formation, cell dehydration and shrinkage, electrolyte disturbance, lipid-protein denaturation, thermal shock).
- Indirect cellular injury (e.g. post-thaw microvascular thrombosis, endothelial damage, intravascular sludging, increased inflammatory mediators, reperfusion injury).
- Destruction of the microcirculation is the main factor leading to cell death. Refreezing of thawed region will exacerbate the initial cellular damage caused by ice crystals and the subsequent post-thawing processes.
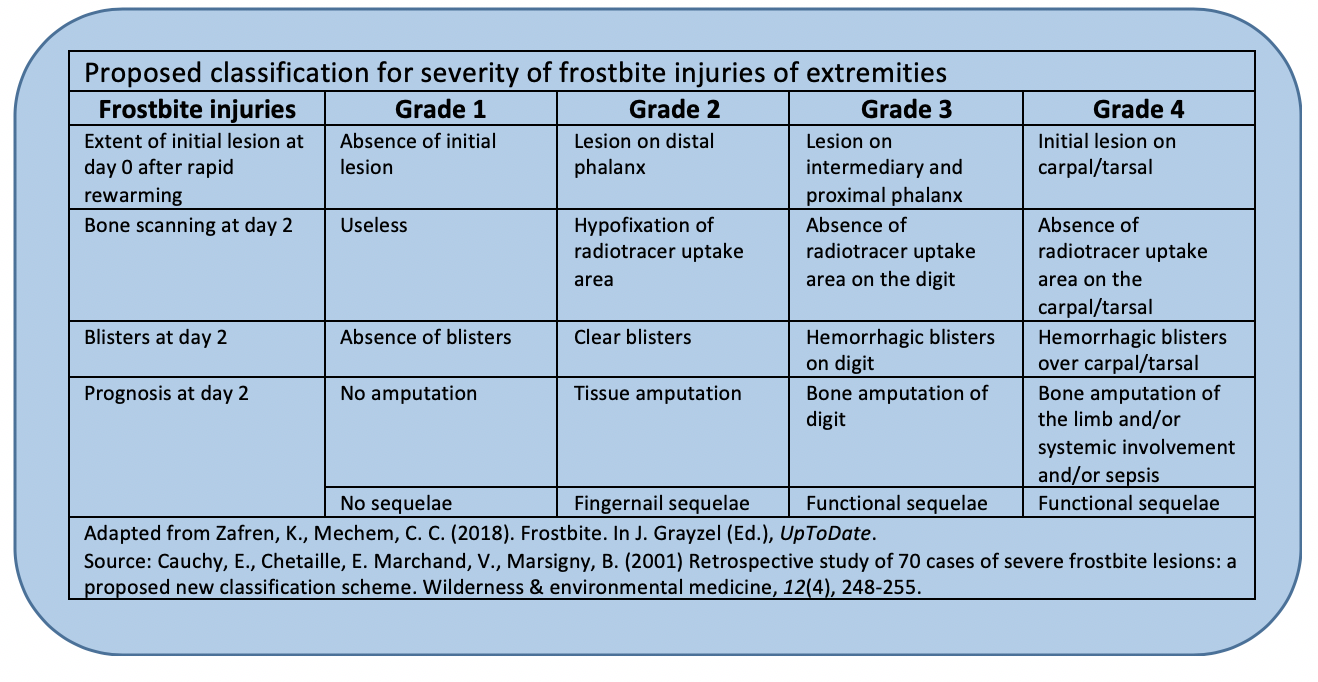
- Traditional Classification of Frostbite (Based upon acute physical findings and advanced imaging after rewarming. Limited prognostic utility):
- First-degree (superficial) frostbite causes numbness and erythema. A white or yellow, firm, and slightly raised plaque develops in the area of injury. No gross tissue infarction occurs; there may be slight epidermal sloughing. Mild edema is common.
- Second-degree (superficial) frostbite injury causes superficial skin vesiculation; a clear or milky fluid is present in the blisters, surrounded by erythema and edema.
- Third-degree (deep) frostbite causes deeper hemorrhagic blisters, indicating that the injury has extended into the reticular dermis and beneath the dermal vascular plexus.
- Fourth-degree (deep) frostbite extends completely through the dermis and involves the comparatively avascular subcutaneous tissues, with necrosis extending into muscle and bone.
Recommended Treatment
Click to view PDF for Deep Frostbite Protocol (for adults)
General Principles:
Treat hypothermia and trauma.
- Rapidly rewarm in water heated and maintained between 37 and 39°C (98.6 to 102.2°F) until area becomes soft and pliable to the touch (approximately 30 min).
Ibuprofen (12 mg/kg per day to a max of 2400 mg/day). Ketorolac IV may increase onset of action compared to oral ibuprofen. - Pain control.
- Tetanus prophylaxis.
- Air dry (i.e. do not rub with towel).
- Debridement: selectively drain (e.g. needle aspiration) clear blisters and leave hemorrhagic blisters intact.
- Topical aloe vera every 6 hr with dressing changes.
- Dry, bulky dressings.
- Elevate the affected area if possible.
- Systemic hydration titrated to maintain normal urine output.
Specific Treatments (consult plastic, general or vascular surgery):
- Thrombolytic therapy: consider for deep frostbite (3rd and 4th degree) at the distal interphalangeal joint or proximal if less than 24 hr after thawing; use angiography for prethrombolytic intervention and monitoring of progress. Consider intravenous thrombolysis if angiography is not available.
- tPA dose is typically a 3 mg bolus (30 mL of 0.1 mg/mL solution) followed by infusion of 1 mg/mL (10 mL/hr) until specialists (eg, vascular, burn, radiology) recommend discontinuation. Heparin is administered concurrently: 500 units/hr.
- Intra-arterial angiography or IV pyrophosphate scanning should be used to evaluate the initial injury and monitor progress after tPA administration as directed by local protocol and resources.
- Prostacyclin (vasodilator) therapy: consider for deep frostbite to or proximal to the proximal interphalangeal joint, within 48 h after injury, especially if angiography is not available or with contraindications to thrombolysis:
- Iloprost IV infusion at a dose 0.5 ng/kg per minute, increased every 30 minutes by 0.5 ng/kg per minute on days 1 through 3, to a maximum of 2 ng/kg per minute. If the patient develops headache or hypotension, the dose is decreased by 0.5 ng/kg per minute. For days 4 to 5, start directly at highest/optimum rate up to 2 ng/kg per minute. Throughout all 5 days, the infusion is given for 6 hours/day at the maximum tolerable rate, up to 2 ng/kg per minute.
- Clinical examination (plus angiography or technetium-99 bone scan if necessary) to assist determination of surgical margins. Evaluation by an experienced surgeon for possible intervention.
Unproven Therapies:
- Hyperbaric oxygen
- Pentoxifylline
- Heparin without thrombolysis
- Other vasodilators
Criteria For Hospital Admission
Admission will depend on the severity of the injury (e.g. deep frostbite), coexisting injuries (e.g. significant swelling), comorbidities, and need for hospital-based interventions (e.g. tPA, vasodilators, surgery) or supportive therapy, as well as ease of access to appropriate community medical and nursing support.
Criteria For Transfer To Another Facility
Dependent on local guidelines.
Criteria For Close Observation And/or Consult
- Early surgical consultation is recommended in frostbite due to possible long-term wound care, tissue debridement, fasciotomy, and delayed amputation.
- Remember attempts at early clinical assessment for tissue viability via the traditional frostbite classification has poor accuracy and progressive changes in the clinical appearance are to be expected.
Criteria For Safe Discharge Home
- Discharge is acceptable if there is no suspicion for any of the previous admission criteria.
- Patients with superficial frostbite can usually be managed as outpatients or with brief inpatient stays followed by wound care instructions.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
The Wilderness Medical Society (WMS) 2019 Practice Guidelines for the management of frostbite are evidence-based.
Related Information
Reference List
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Mar 23, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.