Gastroesophageal Reflux Disease (GERD) – Diagnosis and Treatment
Gastrointestinal
Context
Gastroesophageal Reflux Disease (GERD) affects women and men of all ages. It is one of the most common gastrointestinal diseases worldwide (prevalence ~8-33%) and is the most prevalent acid-related disorder in Canada.
- GERD occurs when gastric contents reflux into the esophagus causing damage or worsening quality of life.
- Patients with GERD report poorer health-related quality of life than those with hypertension, mild diabetes, arthritis or mild heart disease.
- Symptoms are often worse after meals, when bending over, or when laying down.
- 70% of patients with GERD symptoms have normal endoscopy.
- Endoscopy is not required to make a diagnosis of GERD.
- Potential complications of chronic GERD include esophageal stricture, ulcers, Barrett’s esophagus, and esophageal cancer.
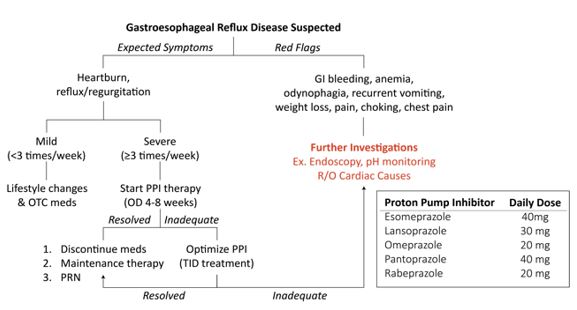
Diagnostic Process
Diagnosed clinically:
- Heartburn ± regurgitation:
- Burning pain in the chest that usually occurs after eating and may occur at night.
- Pain that worsens when lying down or bending over.
- Bitter or acidic taste in the mouth.
- Risk factors: family history of GERD, older age, hiatus hernia, obesity.
- Start PPI trial (once daily for 8 weeks) in patients with suspected GERD who have symptoms more than twice a week. See table below.
Red Flags For Further Investigations:
- Dysphagia, odynophagia, GI bleeding/anemia, recurrent vomiting, involuntary weight loss, chest pain, choking.
- Relapsing, persistent, or atypical symptoms.
- Persistent symptoms despite an adequate PPI trial (4-8 weeks).
- Investigations:
- Consider/rule out cardiac causes.
- Refer for endoscopy and if normal endoscopy, ambulatory pH monitoring.
- Screening for H. Pylori not recommended.
Recommended Treatment
Mild or Infrequent GERD (symptoms less than 3 times per week)
-
- Over-the-counter medications:
- Alginates, antacids, and low dose H2RAs + lifestyle modification.
- Lifestyle modification and education include:
- Weight loss in patients who are overweight.
- Avoid large meals 3h before sleep and elevate the head of the bed.
- Identify and avoid triggers (ie. Smoking, mint, alcohol, carbonated beverages, spicy/acidic foods, chocolate, and caffeine).
- Over-the-counter medications:
Severe or Frequent GERD
-
-
- The above is not effective for the management of severe GERD.
- PPIs are superior to H2Ras for the management of GERD.
- 8-week trial of standard once-daily PPI therapy.
-
- If symptoms resolve, can attempt to discontinue or titrate to the lowest effective dose. Consider an on-demand acid suppression approach for some patients.
- If the inadequate response can try twice-daily PPI therapy for another 8 weeks or change to a different once-daily PPI.
- Not recommended to use prokinetic or promotility agents for initial treatment of GERD.
Created By Ella Barrett-Chan, MSI UBC
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
- Evidence is from the last Canadian Consensus Conference on the management of GERD in adults, which was back in 2004.
Related Information
Reference List
Canadian Consensus Conference on the management of gastroesophageal reflux disease in adults–update 2004.
Armstrong, D., Marshall, J. K., Chiba, N., Enns, R., Fallone, C. A., Fass, R., … & Moayyedi, P. (2005).
– Canadian journal of gastroenterology, 19.Guidelines for the diagnosis and management of gastroesophageal reflux disease.
Katz, P. O., Gerson, L. B., & Vela, M. F. (2013).
– American Journal of Gastroenterology, 108(3), 308-328.Gastro-oesophageal reflux disease and dyspepsia in adults: investigation and management.
ISBN: 978-1-4731-0717-5
– National Institute for Health and Care Excellence (Great Britain). (2014).Advances in the diagnosis of GERD.
Săraru, E. R., Enciu, V., Peagu, R., & Fierbinţeanu-Braticevici, C. (2020).
– Romanian Journal of Internal Medicine, 1(ahead-of-print).
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Dec 10, 2020
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.