Guillain-Barré Syndrome
Cardinal Presentations / Presenting Problems, Infections, Inflammatory, Neurological
Context
Guillain-Barré Syndrome (GBS) is an acute polyneuropathy characterized by immune-mediated peripheral nerve myelin sheath or axon destruction usually in the setting of recent infection.
Heterogeneous presentation, unpredictable course of the disease with wide variation in duration of symptoms and in latency from onset and antecedent infection.
The most common cause of subacute neuromuscular weakness and acute paralysis in North America.
Presentation
- Lower extremity pain and/or paresthesias followed by progressive ascending weakness of lower extremities, and the most severe cases involve respiratory failure and total paralysis.
- Asymmetrical weakness very uncommon.
- Most present days to weeks after resolution of an URTI or GI illness with ascending symmetric weakness or paralysis and areflexia or hyporeflexia.
- Paralysis ascends to level of diaphragm leading to respiratory compromise and requiring mechanical ventilation in one third.
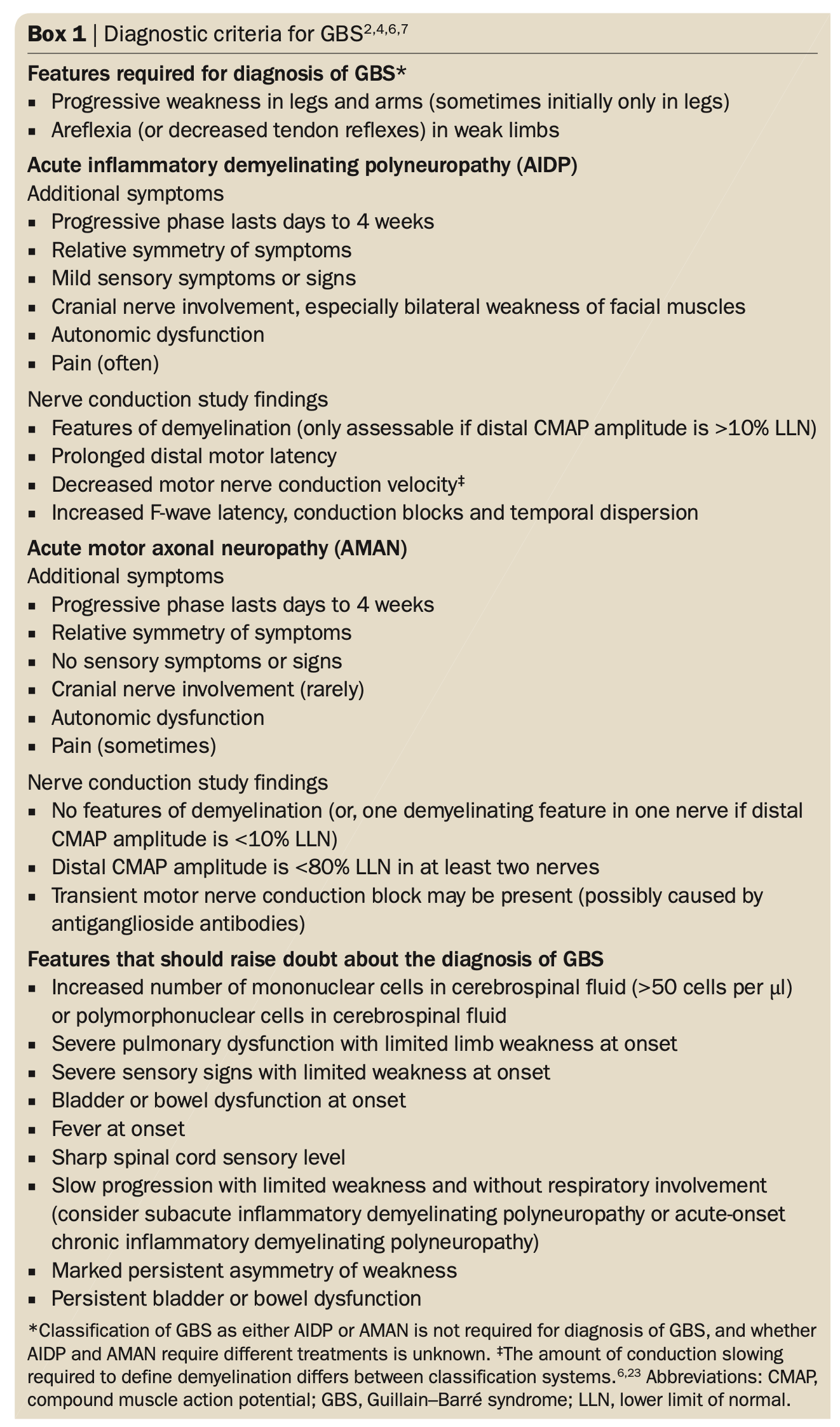
- Many variants exist, with the demyelinating form (acute inflammatory demyelinating polyneuropathy [AIDP]; lymphocytic infiltration of the myelin sheath of peripheral nerves) being common in North America (90% of cases) and the axonal form (acute motor axonal neuropathy [AMAN]; motor paralysis with sensory function intact) being common in Asia or those of Asian descent.
- Cranial nerve abnormalities may be present in about half of patients – bilateral facial weakness, swallowing difficulties, or (sometimes) extraocular motor dysfunction. The Miller-Fisher Syndrome variant (MFS) is characterized by ophthalmoplegia, ataxia, and areflexia, in the absence of extremity weakness.
Pathophysiology
- 2/3 preceded and presumably triggered by infection.
- Cross-reactive antibodies are formed in response to this prior viral or bacterial illness and result in an autoimmune response directed against the myelin sheath and axons of peripheral nerves.
- Campylobacter jejuni is the most common infectious agent associated with GBS.
- Cytomegalovirus (CMV), Epstein-Barr virus (EBV), and Mycoplasma pneumoniae are also associated with development of GBS.
Outcomes
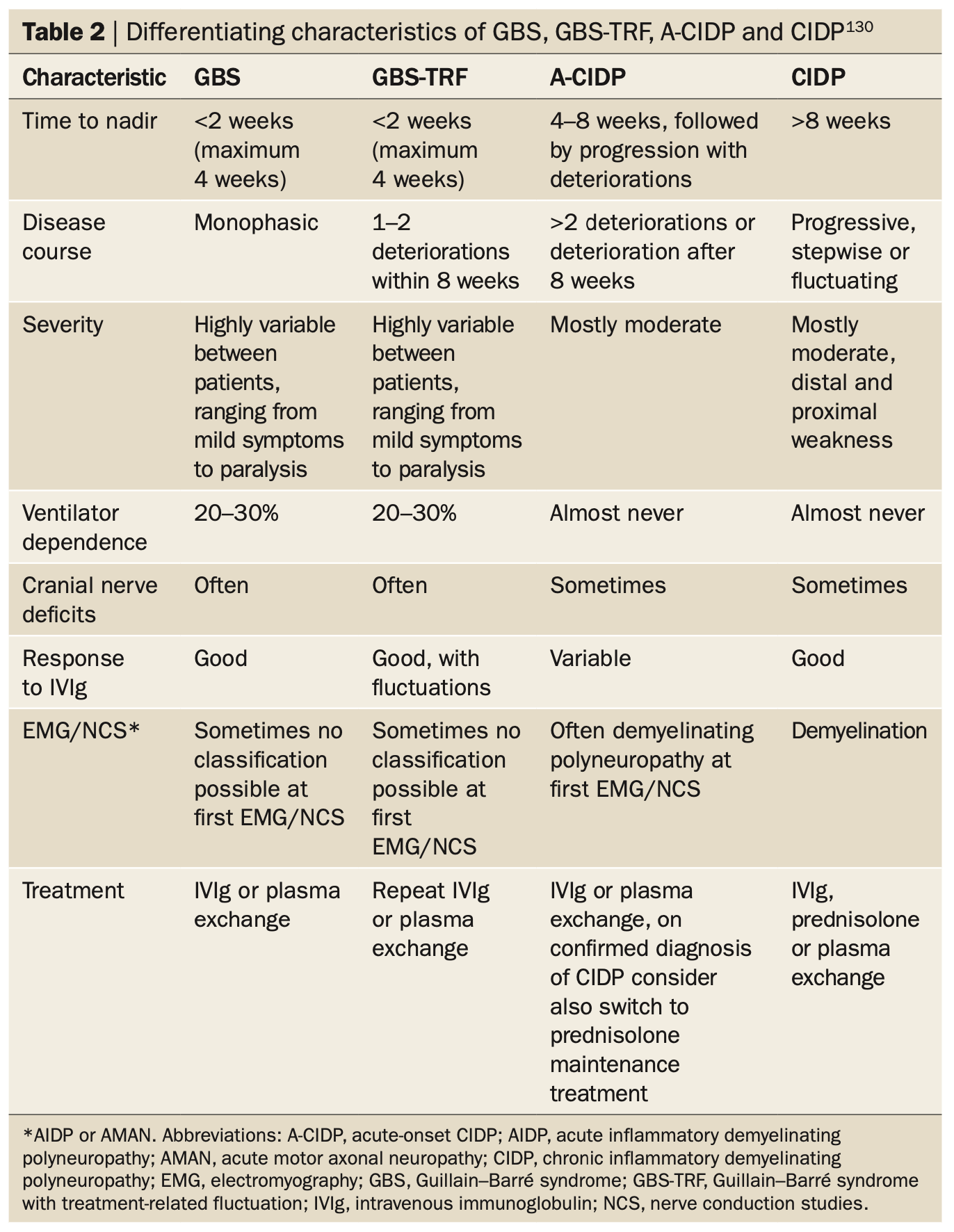
- Symptoms may progress rapidly over hours, reaching a nadir at 2 to 6 weeks (97% <4 weeks), a plateau phase lasting days-months, and lastly recovery, which can vary from weeks to a year or more.
- The majority eventually return to their pre-GBS health status.
- 20% of patients remain disabled from GBS and requiring assistance for ambulation, and about 5% will die despite therapy.
- Recurrence of GBS is rare (<5%), and in rare cases patients may go on to develop chronic inflammatory demyelinating polyneuropathy (CIDP).
Diagnostic Process
Diagnosed mostly by history, and the relatively acute and symmetric nature of symptoms helps distinguish GBS from other illnesses: symmetrical flaccid weakness and decreased reflexes in the absence of alternative causes.
In addition to standard tests:
- TSH
- HbA1c
- Urine for total porphyrins and their metabolites
- Serum/urine delta-aminolaevulinic acid (acute porphyria and lead poisoning all present similarly; abdominal pain, nausea, and neuropathy)
- Porphobilinogen
- HIV
- Titers for Lyme disease (BC CDC website – Borrelia Burgdorferi)
- Skin inspection for a tick bite (tick paralysis)
Detailed neuro exam can localize pathology to peripheral nerves rather than brainstem, brain, spinal cord, NMJ, or muscle itself.
Lumbar puncture
- CSF shows elevated protein without or only slight pleocytosis (albuminocytologic dissociation).
- High protein levels (>45mg/dL).
- WBC counts typically <10 cells/mm3 with predominantly mononuclear cells.
- A normal value cannot be used to exclude GBS: though this is highly specific for GBS, early in the disease patients may have normal CSF values.
When there are >100 cells/mm3 other considerations include HIV, Lyme disease, syphilis, sarcoidosis, tuberculous or bacterial meningitis, leukemic infiltration, or CNS vasculitis.
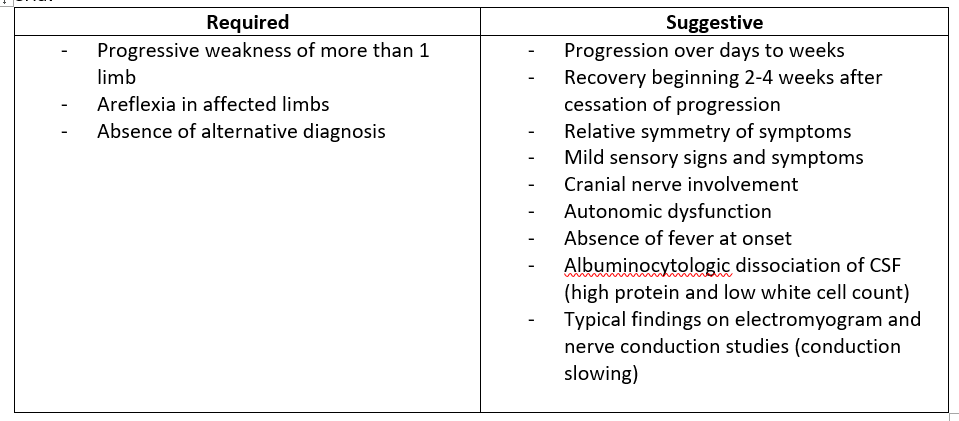
Dx criteria:
Recommended Treatment
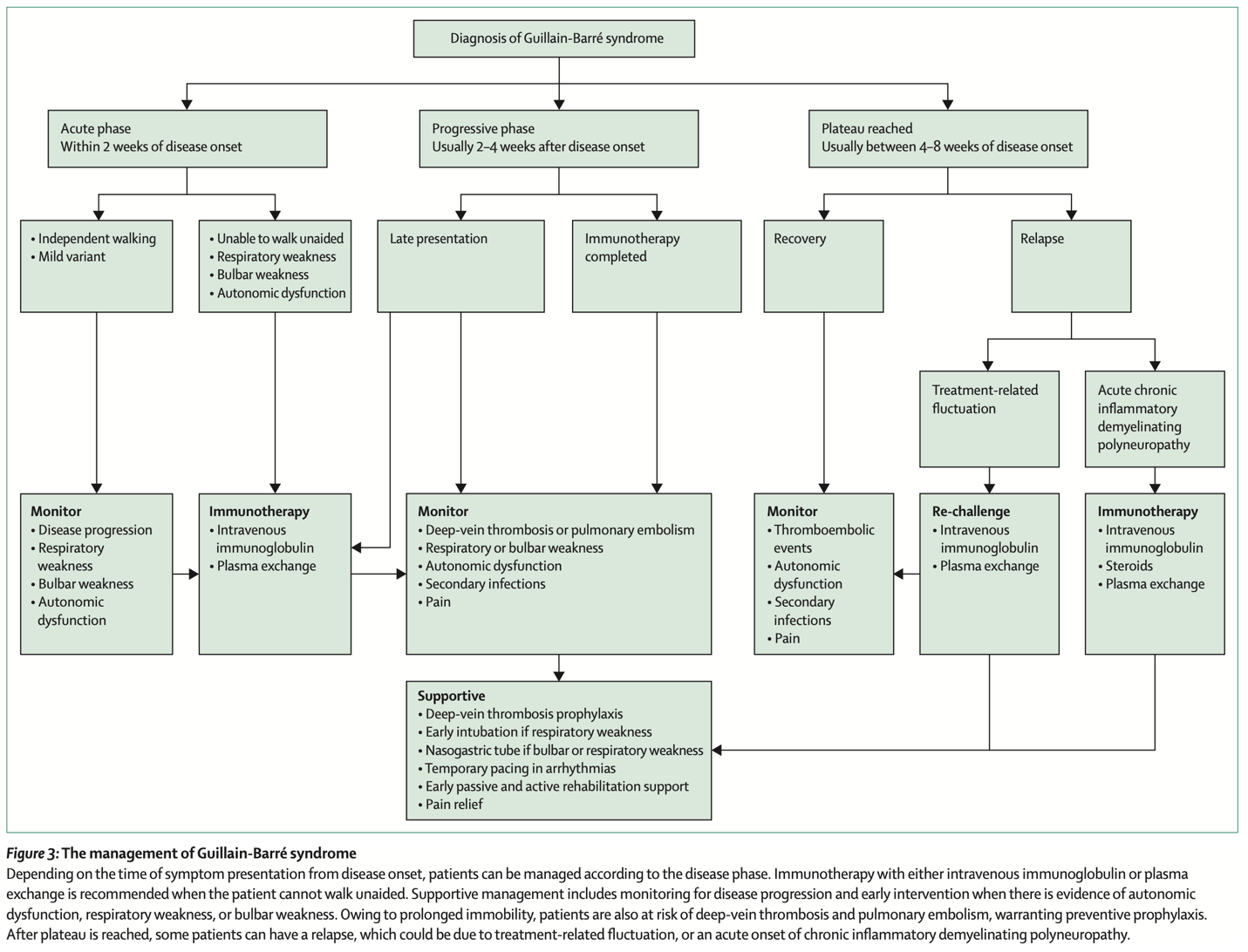
A patient in the progressive phase of GBS requires hospital admission. Admit patients with acute GBS to a unit where cardiac, respiratory, and neurologic functions can be monitored. Even if patient does not initially meet criteria for intubation, ICU admission may still be indicated to avoid sudden, unmonitored respiratory failure.
Assess respiratory function
- Airway protection in advance of respiratory compromise decreases incidence of aspiration and other complications.
- Avoid depolarizing neuromuscular blockers like succinylcholine for intubation in GBS due to risk of hyperkalemic response.
- Patient’s presenting with greater acuity of onset (<1 week) are more likely to develop respiratory failure.
- Tongue weakness has been found to be associated with the development of respiratory compromise and the need for mechanical ventilation in patients with GBS.
- A decreased FVC correlates with need for intubation in patients with GBS.
- Normal is 60-70mL/kg.
- Less than 20mL/kg is associated with pending respiratory failure.
- More than 40mL/kg usually do not require intubation.
- Bedside assessment could be trending values reached when patient counts from 1 to 25 with a single breath.
- FEV1 and PFR can also be used.
Specific treatments
- IV immunoglobulin (IVIG) and plasma exchange (PE; plasmapheresis) shorten the time to recovery.
- Neither is superior.
- Relapse occurs in perhaps 10% of GBS patients after IVIg or PE, a second course of treatment may then be initiated although this has not been proven to be effective.
- IVIG
- IVIG treatment may inhibit Fc-mediated activation of immune cells, binding of antiganglioside antibodies to their neural targets or local complement activation.
- Favored option due to ease of administration and availability.
- PE
- PE is thought to remove neurotoxic antibodies, complement factors and other humoral mediators of inflammation. The largest effect is seen when treatment is started within the first 2 weeks.
- Often not available.
- Corticosteroids
- Corticosteroids of no benefit.
- Combination of IV steroids and IVIG appears to hasten recovery but does not affect long-term outcomes and is not currently recommended.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Related Information
OTHER RELEVANT INFORMATION
Kit’s Journey – a film about a patient’s experience with GBS, filmed at Grey Nuns Community Hospital in Edmonton, AB.
Reference List
GBS/CIDP Foundation International. Guillain-Barré Syndrome: An Acute Care Guide For Medical Professionals. Published online 2012.
Gupta N, Andrus P. Chapter 172: Acute Peripheral Neurologic Disorders. In: Tintinalli JE, Stapczynski JS, Ma OJ, Yealy DM, Meckler GD, Cline DM, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 9th ed. McGraw-Hill Education; 2020:1160-1161.
McGillicuddy DC, Walker O, Shapiro NI, Edlow JA. Guillain-barré syndrome in the emergency department. Annals of Emergency Medicine. 2006;47(4):390-393.
Mirian A, Nicolle MW, Budhram A. Guillain–Barré syndrome. CMAJ. 2021;193(11):E378-E378.
Shahrizaila N, Lehmann HC, Kuwabara S. Guillain-Barré syndrome. The Lancet. 2021;397(10280):1214-1228.
Snow DC, Bunney EB. Chapter 97: Peripheral Nerve Disorders. In: Walls RM, Hockberger RS, Gausche-Hill M, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice. Ninth edition. Elsevier; 2017:1308-1310.
van den Berg B, Walgaard C, Drenthen J, Fokke C, Jacobs BC, van Doorn PA. Guillain–Barré syndrome: pathogenesis, diagnosis, treatment and prognosis. Nat Rev Neurol. 2014;10(8):469-482.
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jun 08, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.