Hyperparathyroidism
Cardiovascular, Critical Care / Resuscitation, Gastrointestinal, Metabolic / Endocrine, Urological
First 5 Minutes
Hypercalcemia crisis (serum calcium > 2.9 mmol/L) can lead to coma and acute renal failure. [1] [2]
Consider Hyperparathyroidism [3] [4]: “Stones, bones, groans, psychiatric overtones.”
- History of kidney stones.
- Bone pain.
- Gastrointestinal Symptoms (constipation, nausea, vomiting, anorexia).
- Confusion, depression, memory loss.
Context
Parathyroid hormone (PTH) maintains serum calcium homeostasis [4].
Normal serum calcium (corrected) = 2.1-2.6 mmol/L [3].
Figure 1. Parathyroid Gland Schematic (https://commons.wikimedia.org/wiki/File:Illu_thyroid_parathyroid.jpg)
Primary Hyperparathyroidism [2] [4] [5] [6]
- Inappropriate secretion of PTH by the parathyroid gland.
- Most common cause of hypercalcaemia.
- Peak age 50-60, male to female ratio 3.5:1.
- Most common in postmenopausal women.
- Risk Factors:
- Prolonged use of furosemide.
- Hx of neck radiation therapy.
- Lithium therapy.
- Causes:
- Adenoma – 85%
- Carcinoma – <1%
Secondary Hyperparathyroidism
- Parathyroid hyperplasia resulting from continual PTH production from low calcium (and high phosphorus).
- Causes:
- Vitamin D deficiency ~ 50%
- Chronic kidney disease (CKD) ~ 15%
- Reduced intestinal absorption (IBD, celiac, surgery)
Diagnostic Process
In the emergency department, identification of severe hypercalcaemia is key.
Figure 2 provides a simplified overview for diagnosis of hyperparathyroidism. Note, Definitive hyperparathyroidism diagnosis not usually established in the ED.
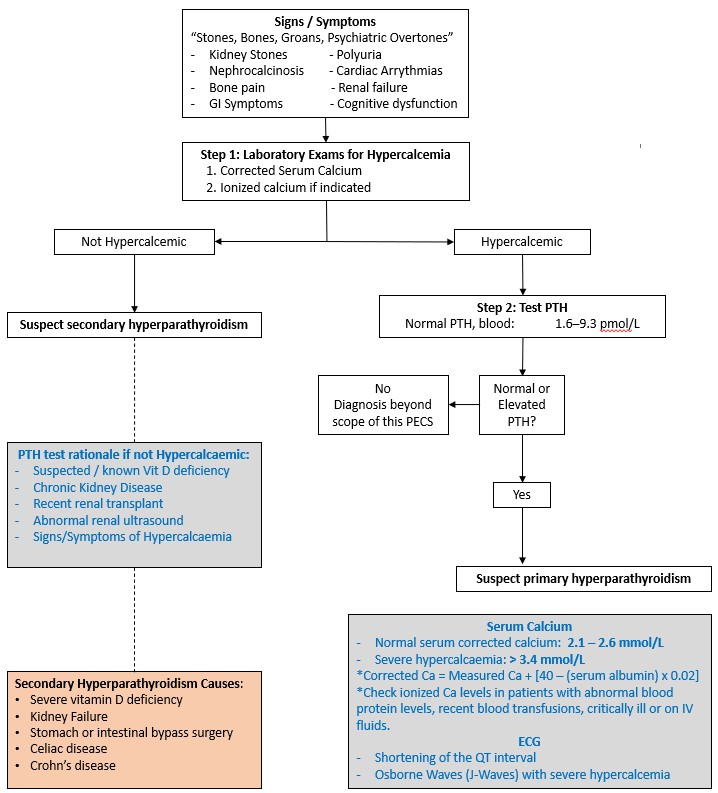
Figure 2. Simplified diagnostic approach for Hyperparathyroidism [2] [3] [4] [7].
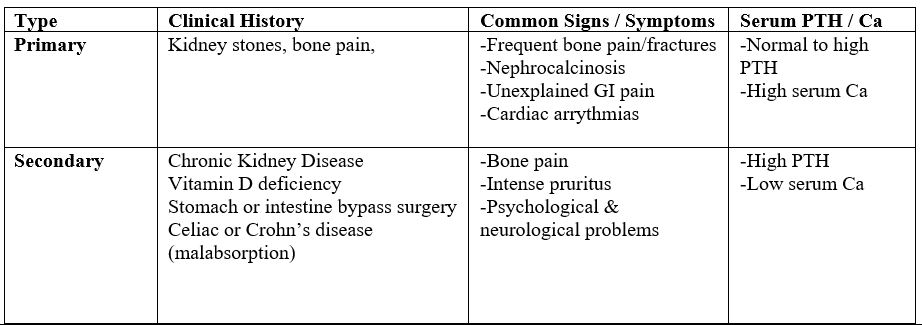
Table 1. Common findings for primary and secondary hyperparathyroidism [2] [4] [7] [8]
Recommended Treatment
Treat hypercalcemia [3]:
- Increase Ca excretion:
- Normal Saline IV Fluids at 200-300mL/hr to promote renal elimination of Ca.
- Loop diuretics, decrease resorption of Ca.
- Hydrocortisone 100mg QID, inhibits effect of Vit D, decrease intestinal absorption of Ca, increase renal elimination of Ca, inhibit osteoclast-activating factor.
- Reduce Ca release:
- Calcitonin lowers Ca within 24-48 hours.
- Bisphosphonates (pamidronate 90mg IV), potent inhibitors of osteoclast activity.
- Others:
- Stop taking drugs that increase Ca, i.e. thiazides, vitamin A and D, and Ca supplements.
- Correct potassium and magnesium level.
The definitive treatment for primary hyperparathyroidism is surgery.
Criteria For Hospital Admission
- Severe hypercalcemia.
- Renal failure.
- Altered mental status.
- Severe dehydration.
- Cardiac complications.
Criteria For Transfer To Another Facility
Acute presentation cannot be managed at the current facility.
Criteria For Close Observation And/or Consult
- Clinically unstable.
- Severe hypercalcemia.
Criteria For Safe Discharge Home
- Clinically stable.
- Follow up possible with Family physician for confirmation or endocrinology.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Risk factors, causes, complications, and treatment of primary hyperparathyroidism are well established. Quality of evidence high.
Due to variable causes, complications and presentations of secondary and other non-PTH mediated forms of hyperparathyroidism, quality of evidence is moderate.
Related Information
OTHER RELEVANT INFORMATION
Reference List
Wallace. Lecture: Parathyroid Basics and Clinical Scenarios in Parathyroid Disease. MEDD 412 2023. Vancouver, British Columbia, Canada: University of British Columbia Medical Program.
Pokhrel et al. Primary Hyperparathyroidism. Retrieved from In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing 2022. https://www.ncbi.nlm.nih.gov/books/NBK441895/
Nickson. Hypercalcaemia. Retrieved from Life in the Fastlane 2020. https://litfl.com/hypercalcaemia/
Taneigra. Hyperparathyroidism. American Family Physician 2004, 69(2), 333-339.
Jamal & Miller. Secondary and Tertiary Hyperparathyroidism. Journal of Clinical Densitometry 2013, 64-68. doi:0.1016/j.jocd.2012.11.012
Melck. Lecture: Endocrine Surgery – Thyroid and Parathyroid. MEDD 412 2023. Vancouver, British Columbia, Canada: University of British Columbia Medical Program.
Muppidi et al. Secondary Hyperparathyroidism. Retrieved from StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing 2023. https://www.ncbi.nlm.nih.gov/books/NBK557822/
Norman Parathyroid Center. Secondary Hyperparathyroidism: Disease of the Parathyroid Glands Caused by Something Else 2023. Retrieved from Parathyroid.com: https://www.parathyroid.com/secondary-hyperparathyroidism.htm
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated May 31, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.