Hypocalcemia
Cardiovascular, Critical Care / Resuscitation, Gastrointestinal, Metabolic / Endocrine, Urological
First 5 Minutes
Consider hypocalcemia for:
- Seizures
- Tetany
- Laryngospasms
- Coma
- Torsades de Pointes
Context
Hypocalcemia is defined as [1]:
- Corrected serum total calcium levels < 2.2 mmol/L
- Ionized calcium 1.17 – 1.33 mmol/L
- Corrected Ca = Measured Ca (mmol/L) + [40-(serum albumin g/L) x 0.02]
New onset hypocalcemia may present to the ED as a life-threatening condition involving multiple organ systems [2].
Common causes [1] [3] [4]:
- Factitious (most common) e.g., low albumin, EDTA blood tube contamination, etc.
- Post-surgical hypoparathyroidism
- Poor dietary intake or malabsorption (Celiac, Crohn’s)
- Vitamin D deficiency
- Acute pancreatitis
- Hyperphosphatasemia
- Hypomagnesaemia
- Hypoparathyroidism
- Congenital / Inherited disorders (e.., DiGeorge syndrome)
- Rhabdomyolysis
- Critical Illness (e.g., sepsis)
- Drugs
- Diuretics
- Beta-blockers
- Phenytoin
- Gentamicin
- Heparin
- Cimetidine
- Ca channel blockers
Most common manifestations of acute hypocalcemia are neuromuscular irritability [2]:
- Paresthesia, numbness, tingling of perioral area, hands or feet
- Carpopedal spasms
- Seizures
- Tetany
- Laryngospasms (rare)
Prolongation of the QT interval can cause cardiac arrythmias [1].
- Torsades of pointes
- Ventricular tachycardia/fibrillation
Coma occurs in 2% of patients, and seizures in 8%. Laryngospasm is rare.
In children 0-5 years old, hypocalcemia leads to potentially life-threatening complications (seizure, arrhythmia, and laryngospasm) in 6.1 per 100,000 patients.
Diagnostic Process
Clinical Hx [1] [5]:
- Paraesthesia’s, numbness or tingling in perioral area, hands or feet
- Muscle cramps
- Seizures
- Tetany
- Syncope
- Diet
- Recent thyroid surgery
- Chvostek Sign
- Trousseau Sign
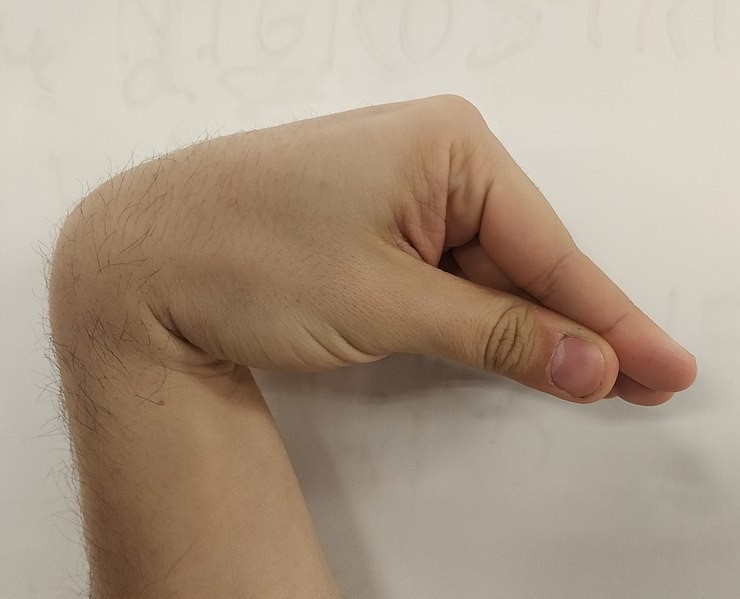
Figure 1. Trousseau’s Sign (https://commons.wikimedia.org/wiki/File:Trousseau%27s_Sign_of_Latent_Tetany.jpg)
Laboratory Exams [1] [4] [6]:
- Corrected serum calcium or ionized calcium
- Normal serum corrected calcium 2.2 – 2.6 mmol/L.
- Mild-moderate hypocalcaemia 1.9 – 2.2 mmol/L.
- Severe hypocalcaemia < 1.9 mmol/L.
- Serum phosphate & magnesium
- Levels should be checked.
- Parathyroid Hormone Levels (PTH)
- If cause not immediately clear.
- Glomerular Filtration Rate (GFR)
- Renal failure may reduce resorption of calcium.
- Associated with high serum phosphate.
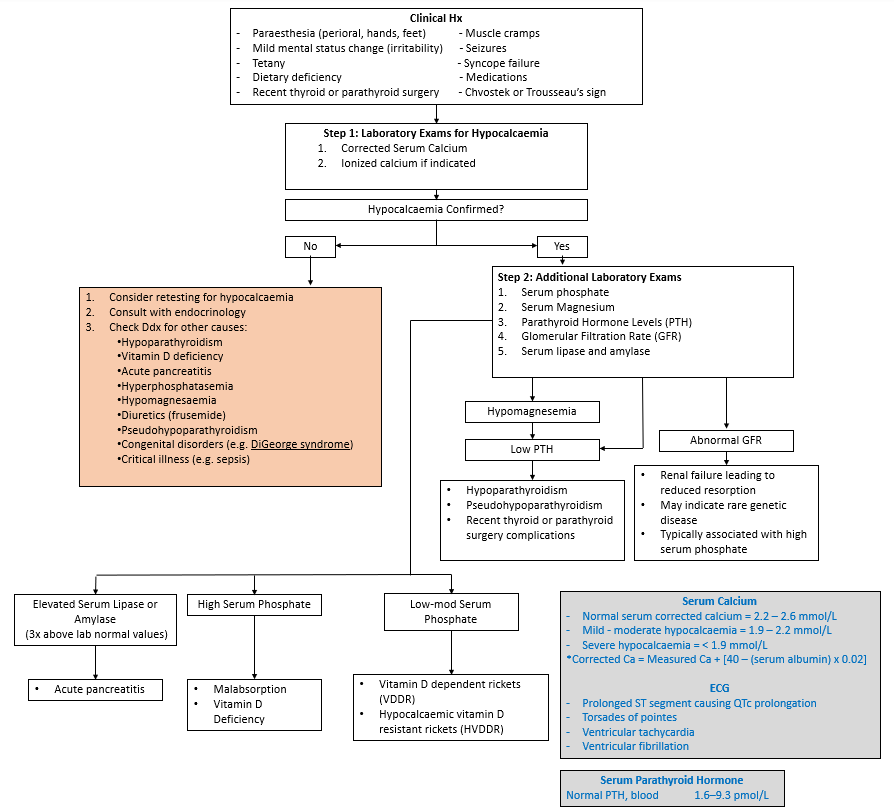
Figure 3. Simplified diagnostic process for new onset or acute hypocalcaemia [2] [1] [5] [4] [6]
Recommended Treatment
Goal of treatment is to raise serum calcium back to normal range [1] [3].
- Treat the underlying cause of hypocalcemia.
- Provide oral or IV Ca therapy.
- Replace magnesium (any efforts to increase serum Ca while hypomagnesemic will not be effective due to magnesium effect on PTH production).
- For suspected chronic, inherited, or other non-acute patients, refer to endocrinology and have followed by family physician.
Mild or asymptomatic hypocalcemia treatment = ORAL calcium [4].
- Indications:
- Mild symptoms e.g., paresthesia
- Asymptomatic
- Administration:
- Use calcium carbonate (40% elemental) or calcium citrate (21% elemental).
- 1500 – 2000 mg elemental Ca per day, divided into 2-3 doses.
- Vitamin D supplementation recommended to promote better Ca absorption.
- In patients taking Proton Pump Inhibitor, don’t use calcium carbonate.
Acute or severe hypocalcemia treatment = INTRAVENOUS Calcium [1] [3] [4]:
- Indications:
- Corrected serum Ca < 1.9 mmol/L or ionized Ca < 0.8 mmol/L.
- Symptomatic hypocalcaemia.
- Hyperkalemia – with cardiac complications (hypotension, dysrhythmias).
- Hypermagnesemia.
- Hypocalcemia with high inotrope requirement.
- Ca channel blocker OD – please see CCB OD Summary.
- Massive transfusion – as per MT protocol.
- Administration:
- Use central line if able and time allows.
- 100 – 300 mg elemental Ca in 100 mL dextrose over 10 – 20 minutes[JM1] [AF2].
- Calcium gluconate: 93 mg elemental Ca / 1g
- Calcium chloride: 273 mg elemental Ca / 1g
- Follow with continuous infusion 0.5-1.5 mg elemental Ca/kg per hour.
- Periodically monitor blood Ca levels until symptoms resolve.
- Monitor with EKG during IV Ca bolus.
- Ca gluconate preferred, less likely to cause tissue necrosis in extravasation [7].
- Contraindications [7]:
- Hypercalcemia, hypersensitivity to calcium gluconate or calcium chloride
- Sarcoidosis.
- In neonates, do not administer with Ceftriaxone.
- In older patients, flush IV lines between administration of Ca and Ceftriaxone.
- Caution in patients with severe hypophosphatemia.
Criteria For Hospital Admission
Acute or severe hypocalcaemia.
Criteria For Transfer To Another Facility
Transfer will depend on local guideline and if acute presentation cannot be managed at the current facility.
Criteria For Close Observation And/or Consult
Confirmed acute or severe cases of hypocalcemia, or when the cause is not known, may be referred to proper specialty service for definitive diagnosis, work-up and treatment.
- Endocrinology
- Internal medicine
Criteria For Safe Discharge Home
- Hypocalcemia complications treated.
- Underlying cause identified or treated.
- Follow-up appointment with specialist or family physician booked (if required).
Context
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Due to variable nature of presentation, causes and treatments, quality of evidence considered low/moderate.
Related Information
OTHER RELEVANT INFORMATION
Calcium Correction Calculator: Calcium Correction for Hypoalbuminemia – MDCalc
Reference List
Burns & Buttner. ECG Library – Hypocalcaemia. Retrieved from Life in the Fastlane 2021. https://litfl.com/hypocalcaemia-ecg-library/
Pepe et al. Diagnosis and Management of Hypocalcemia. Endocrine. 2020, 69(3), 485-495. doi:10.1007/s12020-020-02324-2
Hypocalcaemia DDx. Retrieved from Life in the Fastlane 2023. https://litfl.com/hypocalcaemia-ddx/
Goyal et al. Hypocalcemia. Retrieved from In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing 2022. https://www.ncbi.nlm.nih.gov/books/NBK430912/
Hypocalcaemia. Retrieved from Life in the Fastlane 2020. https://litfl.com/hypocalcaemia/
Pancreatitis. Retrieved from Life in the Fastlane 2020. https://litfl.com/pancreatitis-ccc/
Chakraborty & Can. Calcium Gluconate. Retrieved from In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing 2022. https://www.ncbi.nlm.nih.gov/books/NBK557463/
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated May 31, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.