Hypothyroidism – Diagnosis & Treatment
Metabolic / Endocrine
Context
- Hypothyroidism is the most common hormone deficiency condition and involves insufficient amounts of thyroid hormones produced by the thyroid gland, namely thyroxine (T4) and triiodothyronine (T3).
- Hypothyroidism is more common in women and the incidence increases with age.
- The majority of hypothyroidism cases (~95%) are due to primary hypothyroidism which involves failure of the thyroid gland to produce thyroid hormones.
- Central (secondary or tertiary) hypothyroidism accounts for the remaining 5% of cases and involves impaired secretion of thyroid-stimulating hormone (TSH) from the pituitary gland (secondary hypothyroidism) or impaired secretion of thyrotropin-releasing hormone (TRH) from the hypothalamus (tertiary hypothyroidism).
- Many patients with central hypothyroidism also have deficiencies in other pituitary gland hormones.
Diagnostic Process
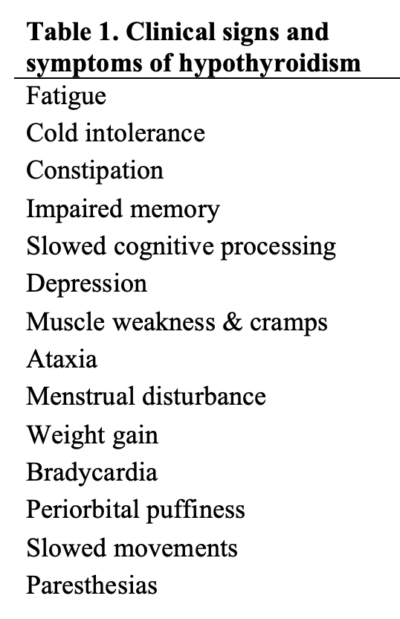
- Due to the nonspecific and variable clinical features of hypothyroidism (Table 1), diagnosis is based on laboratory testing.
Initial Investigation: TSH
- Serum TSH is the first laboratory investigation to order in patients with signs or symptoms of hypothyroidism.
If TSH is elevated:
- Repeat serum TSH measurement
- Measure serum T4:
- If TSH is still elevated and T4 is below the reference range:
- Clinical/overt primary hypothyroidism is suspected
- Initiate thyroid hormone replacement therapy
- If TSH is still elevated and T4 is within the reference range:
- Subclinical/mild primary hypothyroidism is suspected
- Initiation of thyroid hormone replacement therapy on a case-by-case basis
- If TSH is still elevated and T4 is below the reference range:
If TSH is normal or low:
- Repeat serum TSH measurement
- Measure serum T4:
- If TSH is inappropriately normal or low and T4 is below the reference range:
- Central (secondary or tertiary) hypothyroidism is suspected.
- Further investigation and imaging required.
- If TSH is inappropriately normal or low and T4 is below the reference range:
Investigations for Suspected Central Hypothyroidism
- Visual Field defects on exam.
- Suspect if low Free T4and inappropriately low, normal or slightly increased TSH. A delayed TSH response to TRH (TRH stimulation test) supports the diagnosis.
- MRI or Computed Tomography (CT) with coronal views through the pituitary gland (done by consultant).
- Evaluation of other hypothalamic-pituitary-end organ hormones (estradiol, prolactin, gonadotropins, testosterone) in patients with sellar mass lesions on MRI.
- ACTH stimulation test to assess pituitary-adrenal function and adrenal insufficiency.
Recommended Treatment
Thyroid Hormone Replacement
- Initiate levothyroxine (synthetic T4) at a weight-based dose of 1.6 mcg/kg/day in young and otherwise healthy patients.
- Initiate levothyroxine at a lower dose (25 – 50 mcg/day) in patients of older age, with cardiovascular disease, or unknown duration of hypothyroidism.
Disposition
- Admit if hemodynamically unstable, altered mental status, hypothermic, or vulnerable patient.
- If stable to discharge, refer to Internal Medicine, endocrine if no family physician.
Pregnant Patients
- Pregnant women with pre-existing hypothyroidism should increase their dose of levothyroxine by ~30%.
- Pregnant women with newly diagnosed primary hypothyroidism should start levothyroxine at a dose of 1.6 mcg/kg/day to achieve a euthyroid state as soon as possible.
- Endocrine or internal medicine referral.
Untreated Adrenal Insufficiency
- Administration of levothyroxine to patients with untreated adrenal insufficiency may precipitate an adrenal crisis.
- Patients with evidence of central hypothyroidism and other pituitary hormone deficiencies should have pituitary-adrenal function assessed before administering levothyroxine therapy.
Related Information
Reference List
Chaker L, Bianco AC, Jonklaas J, Peeters RP. Hypothyroidism. Lancet. 2017;390:1550-62.
Roberts CGP & Ladenson PW. Hypothyroidism. Lancet. 2004;363:793-803.
Hueston WJ. Treatment of hypothyroidism. Am Fam Physician. 2001 Nov 15;64(10):1717-24
Lania A, Persani L, Beck-Peccoz P. Central hypothyroidism. Pituitary. 2008;11(2):181
-
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Feb 18, 2021
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.