Immunotherapy Checkpoint Inhibitors: What to Know about New Cancer Therapies
Hematological / Oncological
Context
Why should we care?
Checkpoint inhibitors have revolutionized cancer therapy across many organ systems, but they come with novel side effects that are very different from traditional chemotherapies. Emergency physicians need to know what to look for in the acute setting, as these drugs are becoming more widely used for oncology patients.
Immune Checkpoint Inhibitors
- “Immune checkpoints” regulate the immune system response.
- Healthy individual: Checkpoints allow for self-tolerance
- Individual with cancer: Aberrant cancer cells over-express inhibitory checkpoint molecules on their surface to evade immune system.
In brief, checkpoint inhibitors are a type of immunotherapy developed to manipulate the body’s own immune system to fight off cancer cells. Checkpoint inhibitors upregulate the immune system to fight cancer cells.
Checkpoint inhibitors been found to be exceptionally effective in treating an increasing number of cancers, including lymphoma, melanoma, renal cell carcinoma, head & neck, lung cancer… often outperforming conventional cancer therapies. As the rising stars in cancer treatment, checkpoint inhibitors are being studied in almost every type of cancer. It is anticipated that we will see these drugs used increasingly frequently in the cancer patient population.
irAEs’s
What are immune-related adverse events (irAEs), complications of checkpoint inhibitor?
While earlier cancer drugs caused adverse events by compromising defence mechanisms and causing immunosuppression, checkpoint inhibitors have in essence the opposite pathophysiology. They remove some of the normal checks and balances on immune activity to upregulate the immune system to fight cancer cells. As a result, they can induce overwhelming inflammatory responses and autoimmunity in essentially ANY organ system. This can result in autoimmune-like side effects, called “immune related adverse events” (irAEs).
These irAEs can present with varying levels of severity, and it is important for emergency physicians to recognize them. Treatment of irAEs is different from treating side effects of traditional forms of chemotherapy. For each system involved, autoimmune organ dysfunction has been classified and graded into levels of toxicity that emergency physicians should be able to communicate to the on-call BCCA oncologist.
Diagnostic Process
When to consider irAEs
Consider when you see a patient with one of the 6 main cancer types with current Health Canada approval for checkpoint inhibitor therapy. During or after treatment of: Hodgkin’s lymphoma, non-small cell lung cancer, melanoma, renal cell carcinoma, colorectal cancer, head & neck cancer.
More cancer types pending Health Canada approval (HCC, gastric CA)
There are ongoing clinical trials (breast, ovarian, cervical CA, mesothelioma)
Consider when you see a patient with one of the following medications on a patient’s PharmaNet profile:
“-UMAB”
- Ipilimumab (Yervoy) – Anti-CTLA-4
- Pembrolizumab (Keytruda) – Anti-PD-1
- Nivolumab (Opdivo) – Anti-PD-1
- Atezolizumab (Tecentriq) – Anti-PD-L1
Emergency physicians will be able to see the above drugs on their patient’s PharmaNet profile when they present to the ED. This is in contrast to many cytotoxic chemotherapies and other therapeutics which don’t always end up on someone’s PharmaNet profile, so they’re easy to miss. Checkpoint inhibitors are not hidden.
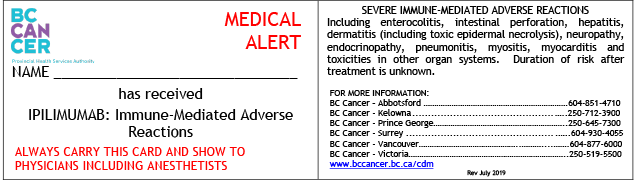
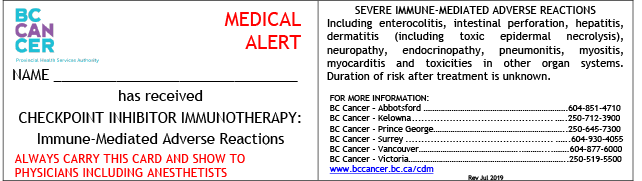
Patients will also be carrying a card in their wallet with the drug name:
CLICK TO DOWNLOAD / PRINT
irAEs Relevant to Emergency Care
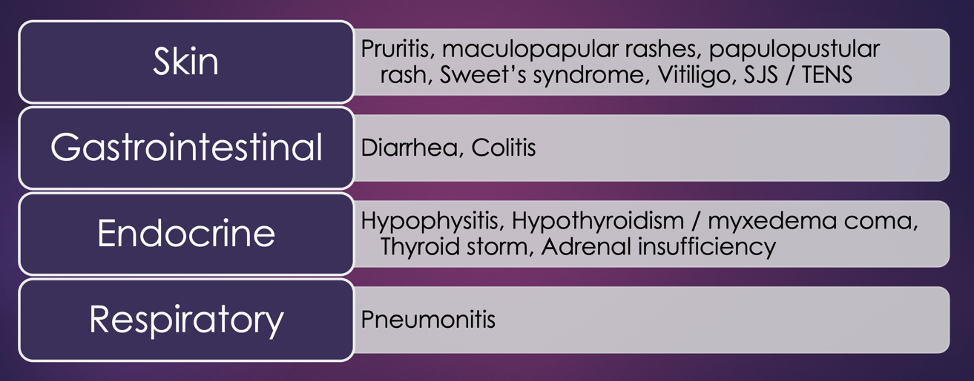
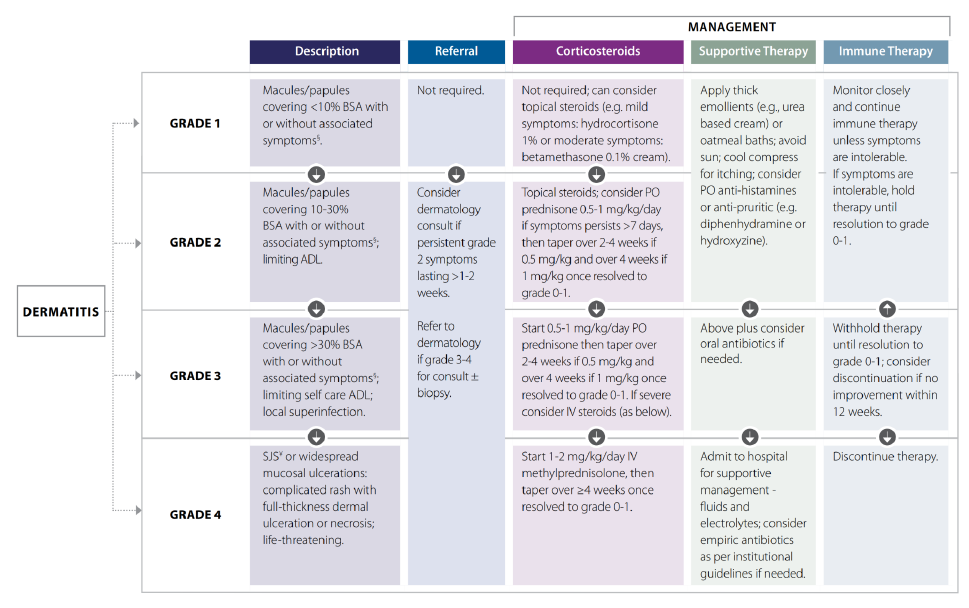
Emergencies involving the skin, the GI system, endocrine, and respiratory system are the most commonly seen in the acute emergency department setting, all of this from retrospective reviews. Diarrhea and colitis are the most common.
- Autoimmune dermatitis can look as benign as eczema, viral exanthems, or cellulitis, but they can also present like SJS or TENS in severe cases
- Diarrhea is very common and happens in up to 70% of patients. Infectious/C-diff work-up should be done as well as abdominal imaging. But when too frequent or combined with abdominal pain, early steroids in this population is critical if considering autoimmune colitis.
- For endocrine adverse events, patients can present with:
- 1) hypo- or
- 2) hyperthyroid,
- 3) adrenal insufficiency, and
- 4) hypophysitis
- at any point after exposure to checkpoint inhibitors.
- Since these have often the most vague and non-specific symptoms, guidelines suggest having a low threshold for considering endocrine problems.
- Respiratory distress from pneumonitis occurs in up to 4% of patients receiving checkpoint inhibitor therapy, most commonly presenting with cough or dyspnea or chest pain.
For each organ system that is affected, emergency physicians can look up on the BCCA website that organ system and use a standardized grading system to assess the severity.
Of patients on checkpoint inhibitors, 70-85% of patients will have some form of irAEs. They are so common that most are managed as an outpatient by oncologists and family physicians. Up to 40% develop severe, life-threatening, or even fatal (grade 3, 4, or 5) events.
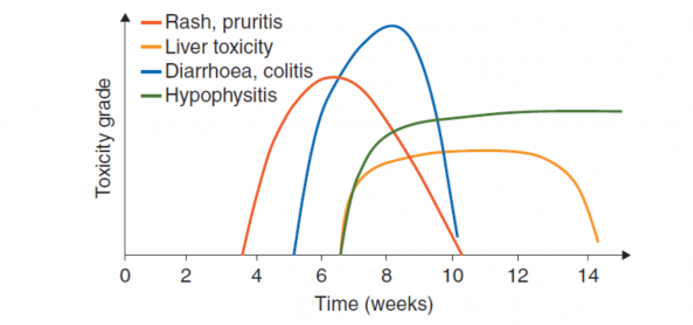
While certain irAEs are more frequent earlier on in the course of treatment and at specific timeframes, in practice they present ANYTIME – from after 2 weeks or 2 years of taking the checkpoint inhibitors, or even 6 months after discontinuing the therapy.
Recommended Treatment
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Related Information
OTHER RELEVANT INFORMATION
Reference List
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Mar 11, 2021
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…



POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.