Influenza
Infections
Context
- Influenza is common and causes a significant burden of disease in the ED.
- Average of 12,200 hospitalizations and 3,500 deaths per year in Canada (1–3).
- Multiple strains of Influenza A and B virus mutate from season to season.
- Influenza A is the most common and most likely to cause epidemics.
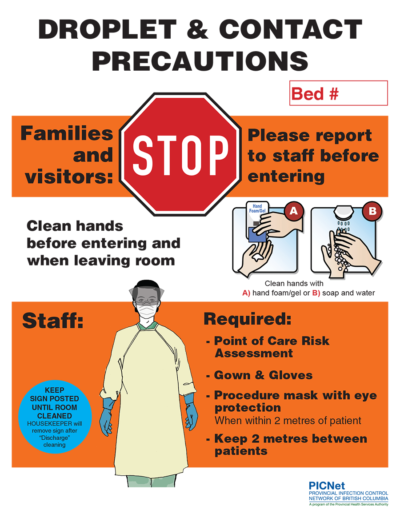
- Transmitted by respiratory secretions – droplet and contact precautions.
CLICK TO DOWNLOAD POSTER
 Source: Provincial Infection Control Network of BC
Source: Provincial Infection Control Network of BC
Clinical Presentation
- World Health Organization defines Influenza-like illness (ILI) as: “An acute respiratory illness with a measured temperature of ≥ 38 °C and cough, with onset within the past 10 days” (5).
- Other typical symptoms include headache, myalgias, malaise, sore throat, rhinorrhea, weakness, dizziness and anorexia.
- Incubation: 18-72 hours.
- Duration 2-5 days; can last more than 1 week.
- Viral shedding 7 days; prolonged in children and immunocompromised.
Complications
- Pneumonia (bacterial or viral)
- NB Community-Acquired – MRSA pneumonia – usually severe.
- Sepsis can be caused by influenza or secondary bacterial infection
- Consider treatment for sepsis if clinically suspected, signs of organ failure, unclear diagnosis.
- Myositis, rhabdomyolysis
- Myocardial infarction, pericarditis, myocarditis
- Encephalitis, aseptic meningitis
- Guillain-Barré Syndrome
- Toxic shock syndrome (Usually Staph aureus).
Management
Isolation
- Droplet and contact precautions.
Personal protective equipment
Supportive management
- Acetaminophen and NSAIDs if no contraindications
- Hydration
- Oxygen as needed.
Specific treatments
- Lung protective ventilation for acute respiratory distress syndrome (ARDS)
- Antibiotics for pneumonia, sepsis, Toxic Shock syndrome
- Antiviral medications (Oseltamivir).
Antivirals
- Consider antivirals in any patient with ILI and symptoms < 48 hours and negative COVID testing.
- Strongly consider treatment regardless of symptom duration of patients with:
- severe influenza (ARDS, pneumonia, hospitalized, cardiac or CNS involvement)
- high risk for severe influenza (Appendix 2).
- Antiviral medications:
- Oseltamivir (Tamiflu) is currently the only option
- Baloxavir marboxil is not yet approved in Canada
- Amantadine is not recommended due to high incidence of resistance.
Testing
- Routine testing for influenza is not indicated.
- Clinical diagnosis is as reliable as laboratory testing for influenza (9).
- Test:
- Patients with severe disease (hospital or ICU admission)
- Unclear diagnosis when testing may decrease antibiotic use or alter further workup
- Most routine testing for influenza in BC is by the viral nasopharyngeal swab (image).
- Nasopharyngeal Swab Video.
Prevention
- Vaccination is the best way
- Hand hygiene
- Respiratory (droplet) precautions
Influenza Vaccination
- Free in BC to high risk people and those in close contact with high risk people (majority of the population)
- Inactivated Influenza (Flu) Vaccine – HealthLink BC
- Offer a flu shot to unvaccinated ED patients as we found 83% were found to be at high risk of influenza complications at Vancouver General Hospital (10)
Related Information
Reference List
Relevant Resources
RELEVANT RESEARCH IN BC
Sepsis and Soft Tissue InfectionsRESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Oct 05, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (2)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.