Intrauterine Device (IUD) Complications
Obstetrics and Gynecology
First 5 Minutes
- Many IUD-related complications present with vague symptoms including abdominal pain and irregular vaginal bleeding. Ask directly about the presence of an IUD as patients may not disclose this without being prompted.
- Consider uterine perforation in a patient who present with abdominal pain and/or abnormal vaginal bleeding when an IUD is in situ.
- A “lost” IUD is an expelled IUD until proven otherwise. Offer back-up contraception for the duration of a pregnancy work-up.
- Consider ectopic pregnancy in a patient with a beta-HCG above 25mlU/mL and an IUD.
- In a systematically unwell patient with an IUD consider sepsis, especially if there is a history of sexually transmitted infection.
Context
- IUDs are T-shaped devices, inserted through the cervix, that can be used for 3-12 years.
- IUDs are 99% effective in preventing pregnancy.
- IUDs come in hormonal, levonorgestrel-containing formulas (Jaydess, Kyleena, and Mirena) and copper formula.
- Serious complications associated with an IUD are rare (<1% occurrence)
- IUD-related complications include:
- Expulsion and the “lost” IUD
- Most common complication and primary IUD-related presentation in the emergency department.
- Expulsion is most common in those who receive an IUD in the early postpartum period (first three days).
- Uterine perforation
- Primary occurrence is at the time of insertion or soon after.
- Increased risk when the IUD is inserted in the postpartum period (up to one year) and among those who breastfeed.
- May be asymptomatic or present with abdominal pain and/or abnormal vaginal bleeding.
- Pelvic Inflammatory Disease (PID)
- Risk is highest in the first 20 days post-insertion and correlates to Neisseria gonorrhea and Chlamydia trachomatis status prior to insertion.
- Concurrent pregnancy
- IUDs decrease the rate of ectopic pregnancies overall, but if an individual has an IUD in situ and is pregnant, the pregnancy is likely ectopic.
- Irregular vaginal bleeding & pelvic pain
- More common with the copper IUD vs hormonal formulations.
- Expulsion and the “lost” IUD
Diagnostic Process
- Expulsion and the “lost” IUD
-
- Risk factors for expulsion include IUD insertion within the first 8 weeks postpartum, and insertion in breastfeeding individuals.
- Consider uterine perforation, especially if presenting with abdominal pain/abnormal vaginal bleeding.
- Attempt to visualize strings using a speculum, if unsuccessful use a cytobrush to sweep the endocervical canal and direct the strings out of the cervix. If still unsuccessful, use ultrasound to assess IUD location.
- Beta-HCG to assess pregnancy status.
- Uterine perforation
- Patient will likely present with abdominal pain and/or abnormal vaginal bleeding.
- Most common with insertion or soon after.
- Ultrasound or laparoscopy to assess IUD location and degree of perforation.
- Assess hemoglobin if patient presents with excessive bleeding, and beta-hCG if uterine instrumentation is indicated.
- PID
- History of Neisseria gonorrhea or Chlamydia trichomonas infection (particularly at time of insertion).
- Presents with lower abdominal pain, cervical motion tenderness, and abnormal vaginal discharge.
- Speculum exam to evaluate mucopurulent discharge.
- Work-up includes: beta-hCG, microscopy of vaginal discharge, NAAT for trachomatis, Neisseria gonorrhoeae, and Mycoplasma genitalium, HIV screening, serologic testing for syphilis.
- Concurrent pregnancy
- Positive pregnancy test.
- Pelvic ultrasound to determine the location of the pregnancy and the IUD.
- Irregular vaginal bleeding & pelvic pain
- More common with the copper IUD.
- Ask about timing of IUD insertion as irregular bleeding may persist for the first six months post insertion.
- Assess hemoglobin if bleeding is excessive.
- Consider ectopic pregnancy.
Recommended Treatment
- Expulsion and the “lost” IUD
- Consider the IUD expelled and provide back-up contraception for the duration of the work-up.
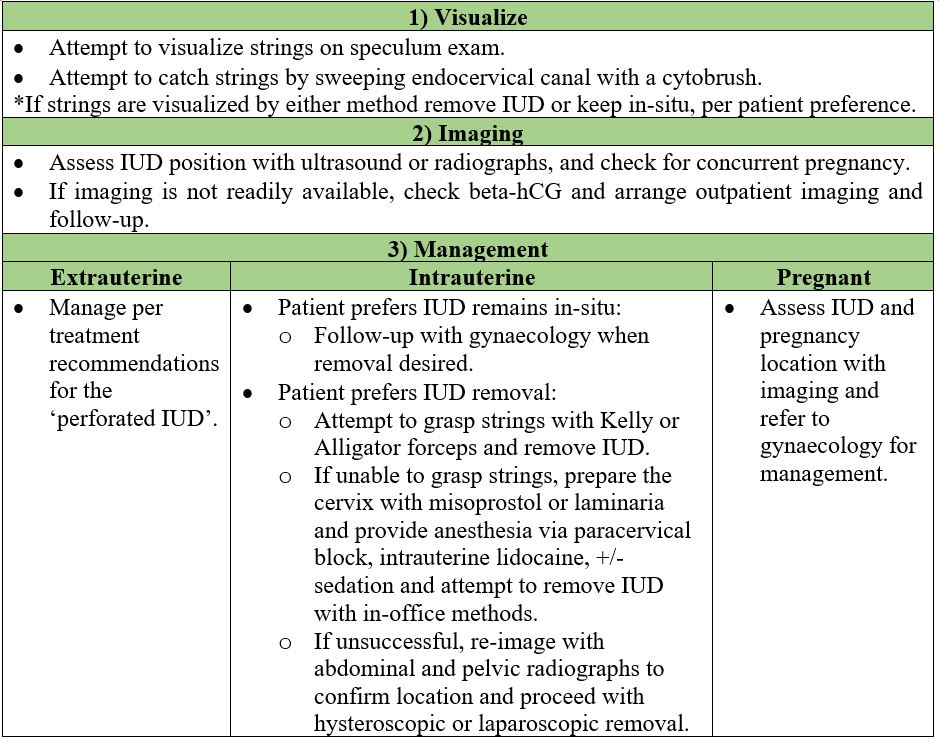
- Follow the steps outlined in table 1.
- Uterine perforation
- Management varies based on the degree of perforation.
- Partially perforated myometrium or embedded IUD (IUD not perforated beyond the serosa):
- Transcervical removal under ultrasound guidance with alligator forceps and a paracervical block for pain management.
- IUD perforated or embedded past the serosa, or completely perforated IUD:
- Deeply embedded IUDS will require an operative hysteroscopy.
- If the IUD is perforated past the serosa, or is completely perforated, intra-abdominal surgery is indicated.
- Asymptomatic patients with a perforated IUD and no other complications (e.g. bowel perforation) may forgo surgery indefinitely.
- PID
- Treat with the IUD in place.
- Concurrent pregnancy
- Management varies based on location of pregnancy.
- Ectopic pregnancy with IUD in situ:
- Leave a properly positioned IUD in place if the ectopic pregnancy can be managed surgically or medically without uterine aspiration.
- Remove a mal-positioned IUD as it may be ineffective for contraception.
- Intrauterine pregnancy with IUD in situ:
- If the pregnancy is not desired, remove the IUD prior to medical or surgical abortion.
- If the pregnancy is desired, remove the IUD in the first trimester if able to do so without uterine instrumentation (e.g., remove if IUD strings are visible or IUD is in the cervical canal; do not remove if the IUD is above the cervix and no strings are visible), otherwise manage the pregnancy with IUD in situ. Removal of the IUD can be done in the ED, or by the primary care provider after consent from the patient. if the IUD is not visible, refer to gynaecology.
- If the pregnancy is not desired, remove the IUD prior to medical or surgical abortion.
- Irregular vaginal bleeding & pelvic pain
- Consider early IUD removal.
Criteria For Hospital Admission
- A complete uterine perforation, while rare, requires urgent treatment.
- A patient found to have an ectopic pregnancy requires admission and prompt treatment.
- A septic patient requires admission.
Criteria For Transfer To Another Facility
- For all IUD-related complications transfer to another facility if unable to properly manage in a timely manner (e.g., a perforated IUD, ectopic pregnancy, or sepsis)
- Ensure patient is stable and consider urgency of treatment and time involved
Criteria For Close Observation And/or Consult
- For all IUD-related concerns, consult obstetrics and gynaecology if the complication cannot be managed in the emergency department (e.g., ectopic pregnancy, perforated IUD).
Criteria For Safe Discharge Home
- Consider follow-up with obstetrics and gynecology or the patient’s general practitioner.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
There is consensus in the literature on complications related to intrauterine devices with little variation between studies.
Related Information
OTHER RELEVANT INFORMATION
SOGC statement on IUDs: https://www.sogc.org/common/Uploaded%20files/Latest%20News/Statement_on_Intrauterine_Devices-E.pdf
Video outlining procedures for complicated IUD removals: https://www.acog.org/programs/long-acting-reversible-contraception-larc/video-series/removal/complicated-iud-removal
Reference List
Myo MG, Nguyen BT. Intrauterine Device Complications and Their Management. Curr Obstet Gyencol Rep. 2023; 12(88-95). https://doi.org/10.1007/s13669-023-00357-8
Prabhakaran S, Chuang A. In-office retrieval of intrauterine contraceptive devices with missing strings. Contraception. 2011; 83(2):102-6. Doi:10.1016/j.contraception.2012.07.004.
Zakin D, Stern WZ, Rosenblatt R. Complete and Partial Uterine Perforation and Embedding following Insertion of Intrauterine Devices. II. Diagnostic Methods, Prevention, and Management. Obstretrical & Gynecological Survey. 1981; 36(8):401. https://journals.lww.com/obgynsurvey/citation/1981/08000/complete_and_partial_uterine_perforation_and.1.aspx
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Oct 26, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.