Leg Swelling: Unilateral and Bilateral – Diagnosis Summary
Cardinal Presentations / Presenting Problems
Context
Edema is defined as a palpable swelling produced by expansion of the interstitial fluid volume which occurs when:
- Movement of fluid from intravascular to interstitial space (Starling’s law)increased capillary
- hydrostatic pressure, and/or
- decreased capillary oncotic pressure, and/or
- increased capillary permeability.
- Retention of sodium and water by the kidneys.
- Interstitial volume must increase by 2.5 to 3L for
- edema to become clinically evident.
Diagnostic Process
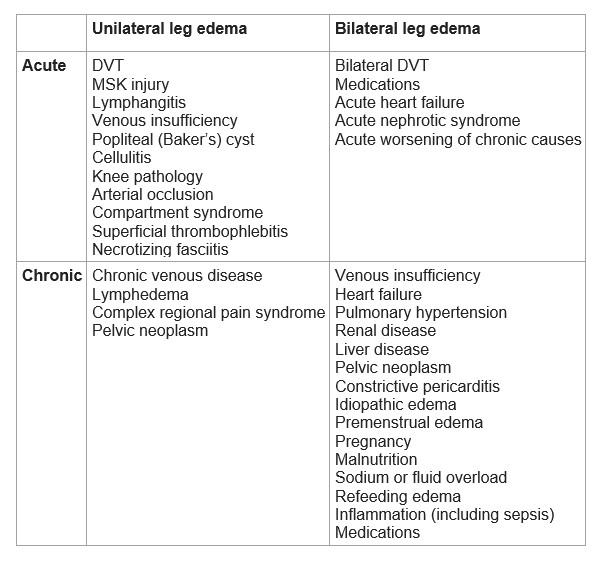
Table 1: Possible etiologies of leg edema in adult patients
Acute unilateral leg edema
Rule out DVT.
DVT work-up is as follows:
Determine pre-test probability for DVT using a scoring system (e.g. Wells score).
- If the pre-test probability is low (Wells score 0-1), then D-dimer can be used to rule out a DVT.
- If pre-test probability is high or D-dimer is positive, then doppler ultrasound of lower extremities is recommended. This is usually done within 24 hrs and the patient is empirically anticoagulated in the meantime.
- Bedside 3-point compression point-of-care ultrasound (POCUS) performed in ED has been shown to have variable sensitivity of 88.9-100% and specificity of 75.9-100% in diagnosing DVT.1 This is in part due to a significant operator learning curve. Decision-making based on POCUS DVT exams should take into account the pre-test probability of DVT, operator experience, and likely include close follow-up.
- Once DVT is ruled out, consider:1,2,3
- 40% – Muscle strain, tear, or twisting injury to the leg – look for history of injury, signs of bleeding/bruising on clinical exam.
- 26% – Unknown.
- 9% – Leg swelling in a paralyzed limb.
- 7% – Lymphangitis or lymph obstruction.
- 7% – Venous insufficiency.
- 5% – Popliteal (Baker’s) cyst – look for posterior knee pain, knee stiffness, mass behind the knee (with knee in extension), and bruising around the ankle.
- 3% – Cellulitis – look for clinical signs e.g. fever, leg warmth, redness.
- 2% – Knee abnormality – look for pain, inflammation, and swelling of the knee joint.
Chronic unilateral leg edema
- The most common cause of chronic unilateral leg edema is lower extremity chronic venous disease.
- Other causes include:
- Chronic venous disease4 – history of thrombophlebitis, hyperpigmentation, and ulceration.
- Lymphedema – history of an ipsilateral inguinal/pelvic lymph node dissection, or radiation therapy.
- Complex regional pain syndrome4,5,6– pain, edema, alteration in skin color and temperature occurring 4-6 weeks after limb trauma.
- Chronic DVT.
- Anatomic obstruction (mass, May-Thurner syndrome).
If presentation is not consistent with above, or significant change, a compression ultrasound with doppler should be obtained.
- Normal study = either lymphedema or complex regional pain syndrome.
- Abnormal venous flow = lower extremity chronic venous disease.
- Suspect neoplasm when ultrasound is suggestive of pelvic outflow obstruction, especially in patients with constitutional symptoms e.g. weight loss. Further pelvic imaging with venous contrast is recommended in these patients.
Acute bilateral leg edema
- Acute worsening of heart failure is a common cause.
- Other etiologies are rare:
- medications (e.g. dihydropyridine CCBs, vasodilators, hormone therapies),
- acute nephrotic syndrome,
- bilateral DVT (often associated with malignancy).
- First consider/rule out DVT. For those with high pre-test probability of DVT, proceed to doppler ultrasound of the legs to evaluate for DVTs.
- For the remaining patients:
-
- Meds: Review medication history and discontinue medications known to cause edema.
- Heart Failure: Hx; Px; CXR, +/- BNP; +/- Echocardiography, ED POCUS can be helpful.
- Renal disease: Urine dipstick for protein and if positive: urine Protein-Creatinine Ratio (PCR) and serum albumin.
- DVT: D-dimer.
Chronic bilateral leg edema
Chronic venous disease is the most common cause. Skin pigmentary changes, induration, and ulceration are usually evident.
Other causes include:7
- Heart failure – history of CHF, dyspnea, orthopnea, PND, abdominal distention, and fatigue.
- Pulmonary hypertension caused by conditions such as sleep apnea – look for signs and symptoms such as excessive daytime sleepiness, loud snoring, interruptions of breathing while sleeping.
Less common causes include:
- Renal disease
- Liver disease
- Pelvic neoplasm
- Constrictive pericarditis
- Idiopathic edema
- Premenstrual edema
- Malnutrition
Lymphedema and myxedema (e.g. severe hypothyroidism) are not true edematous states.
If initial history and clinical exam are not indicative of the etiologies listed above, consider:
- urine dipstick protein,
- serum creatinine,
- albumin, PT/INR, liver function tests,
- TSH.
If these tests are unremarkable, consider:
- Echocardiogram to evaluate the possibility of heart failure or pulmonary hypertension should be obtained.
- CT pelvis with contrast is recommended to exclude a pelvic neoplasm if all other investigations are negative.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Evidence comes from a wide range of studies addressing the etiology and diagnosis of leg edema that are in relative agreement with each other.
Related Information
Reference List
García, Jorge Pedraza, et al. “Comparison of the accuracy of emergency department-performed point-of-care-ultrasound (POCUS) in the diagnosis of lower-extremity deep vein thrombosis.” The Journal of emergency medicine 54.5 (2018): 656-664.
Hull R, Hirsh J, Sackett DL, et al. Clinical validity of a negative venogram in patients with clinically suspected venous thrombosis. Circulation 1981; 64:622.
Gorman WP, Davis KR, Donnelly R. ABC of arterial and venous disease. Swollen lower limb-1: general assessment and deep vein thrombosis. BMJ 2000; 320:1453.
Chiesa R, Marone EM, Limoni C, et al. Chronic venous disorders: correlation between visible signs, symptoms, and presence of functional disease. J Vasc Surg 2007; 46:322.
Executive Committee of the International Society of Lymphology. The diagnosis and treatment of peripheral lymphedema: 2020 Consensus Document of the International Society of Lymphology. Lymphology 2020; 53:3.
Marinus J, Moseley GL, Birklein F, et al. Clinical features and pathophysiology of complex regional pain syndrome. Lancet Neurol 2011; 10:637.
Blankfield RP, Finkelhor RS, Alexander JJ, et al. Etiology and diagnosis of bilateral leg edema in primary care. Am J Med 1998; 105:192.
Related Information
OTHER RELEVANT INFORMATION
3 point compression POCUS for DVT diagnosis
http://www.emdocs.net/ultrasound-g-e-l-accuracy-of-3-point-dvt-exam/
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jan 19, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (1)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.