Lyme Disease
Cardiovascular, Infections, Neurological, Orthopedic
Context
- Tickborne illness is the most common vector-borne disease in North America.
- Spirochete bacteria Borrelia burgdorferi is transmitted by the Ixodes scapularis (Eastern) and Ixodes pacificus (Western) ticks.
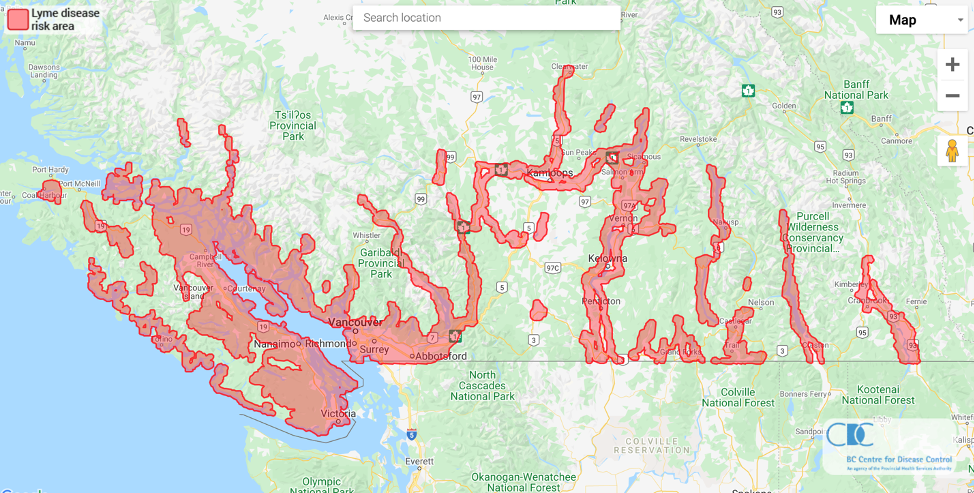
- Lyme disease is found worldwide, with areas of increased risk depending on the prevalence of burgdorferi in Ixodes ticks.
- The majority of Canadian cases are found in Ontario, Quebec, and Maritime provinces, however, Lyme disease is present in all ten provinces.
- The greatest incidence is during spring and summer months, when tick feeding and human outdoor activity peak.
- Transmission generally occurs during feeding after 36-48 hours of attachment, followed by an incubation period of 1-36 days.
- Patients will typically present to the ED in one of two ways:
- With a recent tick exposure and concern regarding prophylaxis.
- With erythema migrans rash or other consistent symptoms and appropriate epidemiologic exposure.
Diagnostic Process
- Diagnosis is primarily clinical but can be augmented with serological testing in specific cases. Chronic Lyme disease may mimic many other chronic conditions.
- Diagnosis can be made when a patient has a possible exposure in a Lyme-endemic area (Figure 1) AND has clinical symptoms consistent with Lyme disease. Many patients with Lyme disease may not recall a tick bite, and such a history is not required to substantiate an “exposure”.
- Clinical findings consistent with Lyme disease are divided into several stages:
- Early Lyme disease
- Non-specific influenza-like illness.
- Erythema migrans rash.
- Early disseminated Lyme disease
- Neurologic: Unilateral or bilateral facial nerve palsy, mononeuritis multiplex, peripheral radiculopathy/neuropathy, lymphocytic meningitis.
- Arthritis: inflammatory asymmetric large joint oligoarthritis.
- Carditis: AV block, myopericarditis.
- Chronic Lyme disease
- Neurologic: Encephalopathy, polyneuropathy.
- Chronic arthritis.
- Post Lyme disease syndrome (after appropriate treatment)
- Non-specific headache, malaise, fatigue, arthralgias, cognitive difficulties.
- Early Lyme disease
- Erythema migrans is the classic dermatological finding associated with Lyme disease (Figure 2). It occurs in up to 90% of patients, though a thorough search of the skin is required. It is a slowly expanding area of erythema that may have associated central clearing (classic “bullseye rash”) and lasts days to weeks. Multiple smaller satellite lesions may occur. Compared to cellulitis, lesions are typically not tender.
- With suspected early Lyme disease (exposure PLUS erythema migrans), serologic testing is not indicated, and treatment should be given.
- With suspected early disseminated or chronic Lyme disease and appropriate exposure history, serologic testing may be useful.
- Consultation with a local infectious disease specialist is recommended.
- Routine laboratory investigations (CBC, CRP, blood/CSF cultures, etc.) low-yield and but may be helpful to exclude other infections.
- Consider testing for additional tick-borne diseases if appropriate, such as Babesiosis and Anaplasmosis.
Recommended Treatment
- Tick bite Lyme disease prophylaxis criteria
- Exposure to a Lyme endemic area (>20% rate of infection with B. burgdorferi in Ixodes ticks).
- Tick engorged or attached for >36h.
- Prophylaxis given within 72 hours of removal.
- The IDSA also recommends that the tick be identified as an Ixodes tick, however, this is impractical and not necessary in most clinical scenarios.
NOTE: The prevalence of B. burgdorferi in ticks in BC is consistently < 1%, and therefore prophylaxis is not indicated for patients with tick exposure within BC even in Lyme disease risk areas (BC CDC). For patients presenting with tick exposure from other Lyme risk areas (E.g. Eastern USA) need for prophylaxis should be assessed based on the local infection rate.
- Tick bite Lyme disease prophylaxis treatment
- Single dose Doxycycline 200mg PO.
- Early Lyme disease treatment (exposure PLUS erythema migrans)
- Treatment with appropriate antibiotic for 10-21 days.
- Doxycycline 100mg PO BID (preferred).
- Amoxicillin 500mg PO TID.
- Cefuroxime 500mg PO BID.
- Treatment with appropriate antibiotic for 10-21 days.
- Note: 15% of patients may have a transient worsening of symptoms after initiating treatment lasting for 1-2 days
Jarisch-Herxheimer reaction which occurs after initiation of antibacterials when treating Gram-negative infections such as Escherichia coli and louse- and tick-borne infections. It usually manifests in 1–3 hours after the first dose of antibiotics as fever, chills, rigor, hypotension, headache, tachycardia, hyperventilation, vasodilation with flushing, myalgias and exacerbation of skin lesions and anxiety. - Early disseminated Lyme disease treatment
- Patients with acute carditis should be treated with IV antibiotics and admitted for cardiac monitoring. Once symptoms are resolving, patients can be stepped down to oral for a total 21-28 day course.
- Ceftriaxone 2g IV daily.
- Alternatives: Cefotaxime, Penicillin G.
- Patients with mild neurologic or arthritic manifestations can be followed as outpatients with oral antibiotics for 14-21 days.
- Doxycyline 100mg PO BID (preferred).
- Amoxicillin 500mg PO TID.
- Cefuroxime 500mg PO BID.
- Patients with acute carditis should be treated with IV antibiotics and admitted for cardiac monitoring. Once symptoms are resolving, patients can be stepped down to oral for a total 21-28 day course.
- Chronic Lyme disease
- Patients with neurologic symptoms should receive a 14-day course of Ceftriaxone 2g IV daily.
- Patients with arthritis or dermatologic features can be treated with a 1-month course of doxycycline 100mg PO BID.
Other Resources
How to Properly Remove a Tick – Video (University of Manitoba YouTube channel)
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Overall evidence in this area is mixed, with some high-quality randomized trials for early Lyme disease treatment, but a relative paucity of evidence for early disseminated and chronic Lyme disease.
Related Information
Reference List
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Oct 20, 2020
Visit our website at https://emergencycarebc.ca
COMMENTS (2)
Add public comment…



POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.